
Moderator of 1 Session
Presenter of 1 Presentation
FLASH: Path to Clinical Translation
Abstract
Abstract Body
FLASH radiation therapy is rapidly progressing to human clinical trials. This presentation will review the preclinical data from the perspective of key questions needed for clinical translation. It will also summarize the technological basis, current and under development, for ongoing and future clinical trials of FLASH radiation therapy.
Author Of 4 Presentations
FLASH: Path to Clinical Translation
Abstract
Abstract Body
FLASH radiation therapy is rapidly progressing to human clinical trials. This presentation will review the preclinical data from the perspective of key questions needed for clinical translation. It will also summarize the technological basis, current and under development, for ongoing and future clinical trials of FLASH radiation therapy.
RAPID CONVALESCENT PLASMA STERILIZATION USING HIGH DOSE RATE ELECTRON RADIATION
Abstract
Background and Aims
Passive antibody administration through convalescent plasma has shown benefit in treating COVID-19 in the early stages of the disease in patients >65 years old, and in other viral outbreaks. A practical, rapid method to sterilize convalescent plasma while also maintaining antibody function would be valuable for safe treatment in future viral pandemics. Plasma sterilization by irradiation requires kGy of dose to deactivate bacteria and viruses of concern. Conventional lab-based irradiators would require days to reach such doses, while ultra-high dose rate irradiation (FLASH) would require minutes. We present a proof-of-concept on sterilizing plasma with 25 kGy in approximately 3 minutes without damaging the antibodies in the plasma.
Methods
A Varian Trilogy LINAC was configured for 16 MeV FLASH electron irradiation. Frozen aliquots of convalescent plasma from patients with COVID-19 were placed in a 3D printed holder submerged in liquid aiming to preserve sample temperature (RT, 4C or -20C). The number of pulses was estimated with EBT-XD film. Samples were irradiated with a dose of 25 kGy in ~33,330 pulses over 185 seconds. Antibody binding against the receptor-binding domain (RBD) of the S1 region of SARS-CoV-2 was measured by ELISA pre- and post-irradiation.
Results
Frozen plasma aliquots from 10 COVID-19 convalescent plasma donors were irradiated in frozen state to 25 kGy dose. IgG antibody binding against SARS-CoV-2 RBD after irradiation remained at 90.8% of non-irradiated samples (Figure; OD 1.25 vs. 1.36, p< 0.0003).
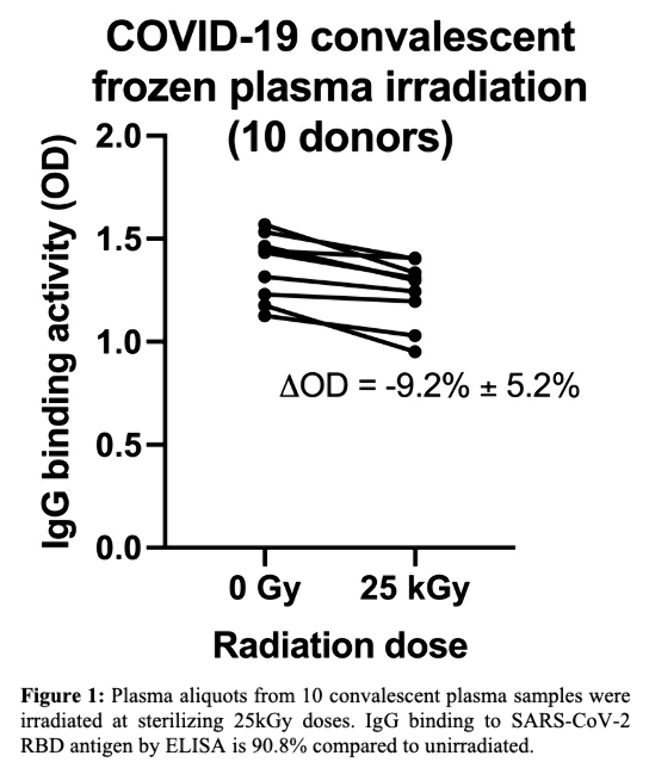
Conclusions
FLASH irradiation allows for rapid sterilization of blood plasma from potential pathogens while largely preserving antibody binding function and specificity.
REAL-TIME OPTICAL OXIMETRY UNDER IRRADIATION
Abstract
Background and Aims
Transient changes in oxygen tension in tissues taking place during FLASH radiotherapy may explain its biological effects. However, because the kinetics of oxygen depletion and recovery occur on a very short timescale, it is challenging to measure these effects in vivo using existing methods. Here we developed a real-time optical oximetry system with millisecond temporal resolution to elucidate early radiochemistry under irradiation.
Methods
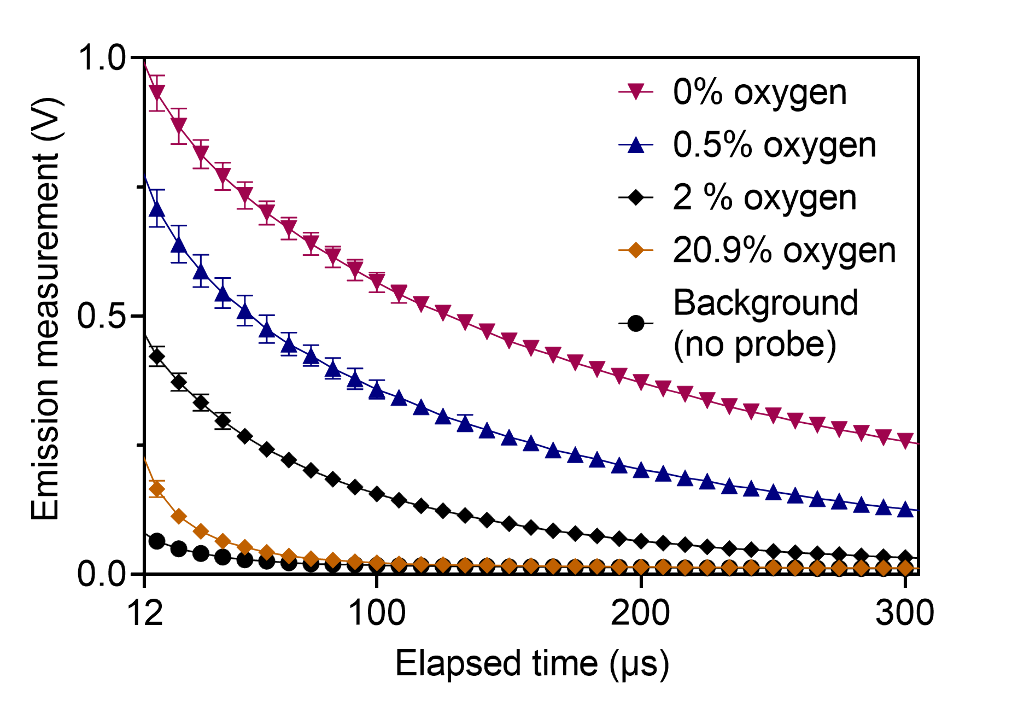
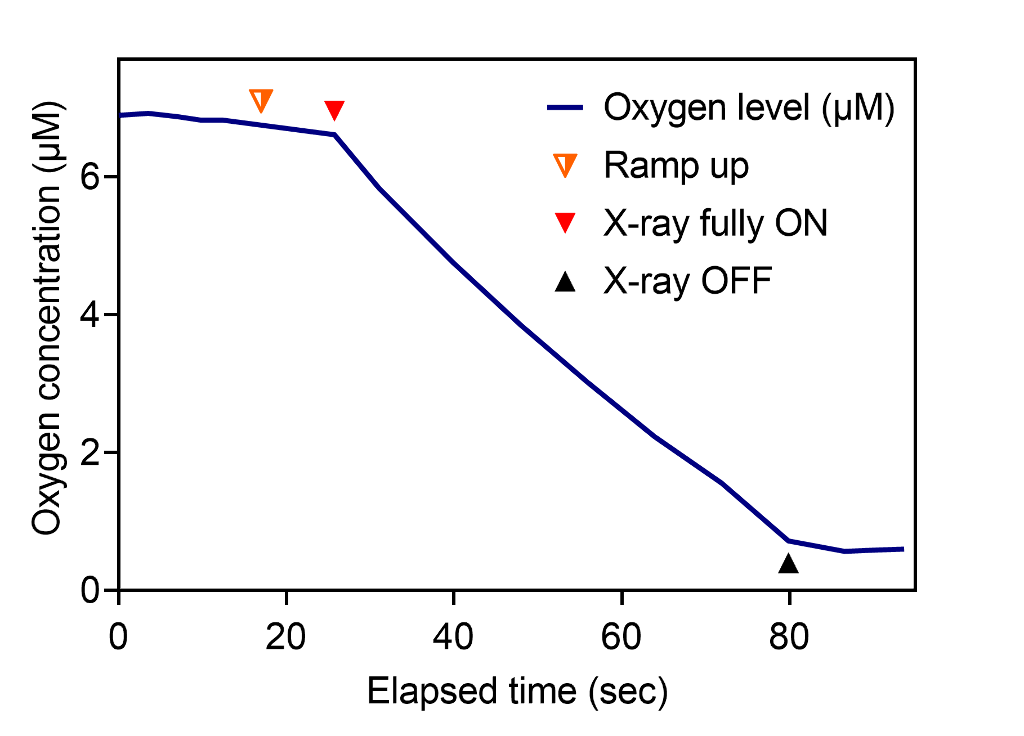
Oxygen measurements were performed in vitro using the phosphorescence quenching method and a water-soluble molecular nanoprobe (Fig. 1). An epifluorescence fiber-coupled system was designed and built. The system was validated using a standard dissolved oxygen meter. The changes in oxygen per unit dose (G-value) were quantified in response to irradiation by 320 kVp x-ray and 16 MeV electron beam at dose rates ranging from 0.04 Gy/s to 100 Gy/s.
Results
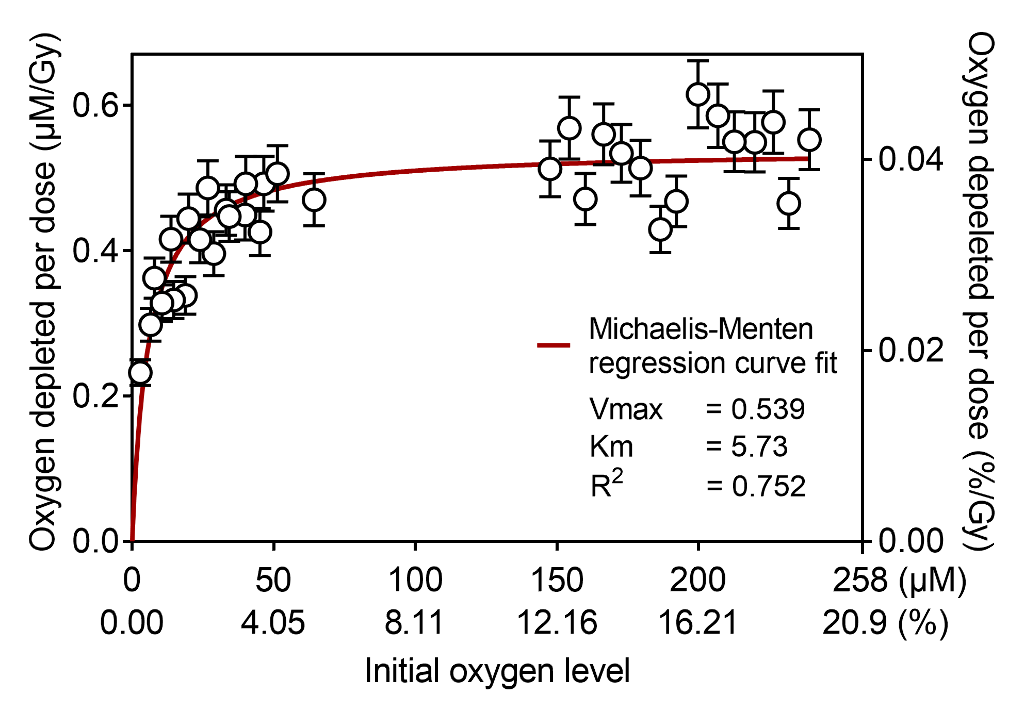
Transient oxygen depletion of phosphate buffer solution under standard kV X-ray irradiation was continuously measured every millisecond (Fig. 2). The samples at normoxia with oxygen concentration of 150–240 µM had constant G-value of 0.54 uM/Gy, however hypoxic samples (15 µM and below) had significantly lower G-values (Fig. 3).
Conclusions
Our observations suggest that oxygen depletion rate decreases under hypoxia, with the measured data being a good fit to Michaelis-Menten kinetics. Future works will measure oxygen depletion kinetics of biomimetic lipid emulsions and in vivo mice under irradiation. We anticipate that the proposed method will capture crucial millisecond-order oxygen change after individual e-beam pulses.
3D HIGH SPEED RF BEAM SCANNER FOR HADRON THERAPY OF CANCER
Abstract
Background and Aims
Treatment of cancer using actively scanned hadron pencil beams (protons and light ions) has major clinical advantages over treatments using photons. However, current methods used to adjust beam energies by degrading the beam are not compatible with the high dose rates needed for FLASH therapy. We are pursuing the demonstration of a compact accelerator technology to rapidly scan the energy and the trajectory of the hadron pencil beam to deposit the desired dose at FLASH dose rates.
Methods
We utilize RF energy modulation and deflection to enable a dose delivery of 50 Gy/L/s. Very fast irradiation presents many benefits to patients: (1) it solves the issue of patient motion and thus removes the need for tracking organ motion during irradiation (motion-adapted radiation therapy); it implies single- or hypofractionated treatments which will (2) increase dramatically patient throughput and (3) present biological benefits.
Results
We will present key innovations for energy modulation and lateral steering, including the design, optimization, and testing of critical components of an RF accelerator, RF deflector, and a PMQ. We have modeled dose deposition in phantoms with realistic beam parameters. We will also present our approach to integrating these technologies at a clinical beamline, monitoring dose deposition on a phantom target, and utilizing this information for treatment planning.
Conclusions
The scanner can be adjusted to cover the depth and lateral extent of the tumor while maintaining the quality of the pencil beam. Scanner operation in a clinical setting will provide definitive proof that the approach is viable and compatible with high dose rate FLASH.

