A. Pareek (Rochester, US)
Mayo ClinicPresenter Of 3 Presentations
12.3.4 - Patient-Specific Survival Prediction of Osteoarthritis in Hip Femoroacetabular Impingement Patients Using Machine Learning
Abstract
Purpose
The purpose of this study is (1) Predict survival curve of progression to OA for individual Hip FAI patient with machine learning algorithm and (2) compare performance of machine learning-based survival model and conventional Cox proportional hazard (CPH) model.
Methods and Materials
Between 2000 and 2016, all patients diagnosed with FAI in the Rochester Epidemiology Project were reviewed. Total of 1,012 patients with a mean age of 28.5 years were included. Demographics, physical exam, imaging features were included. The patient’s data was randomly split into Train (70%) and test (30%) sets.
Random survival forest (RSF), a non-parametric tree-based survival model is used to assess survival curves for individual patient. Concordance probability (C-index), the pairwise probability of lower patient risk given longer survival time, was used for evaluation.
Results
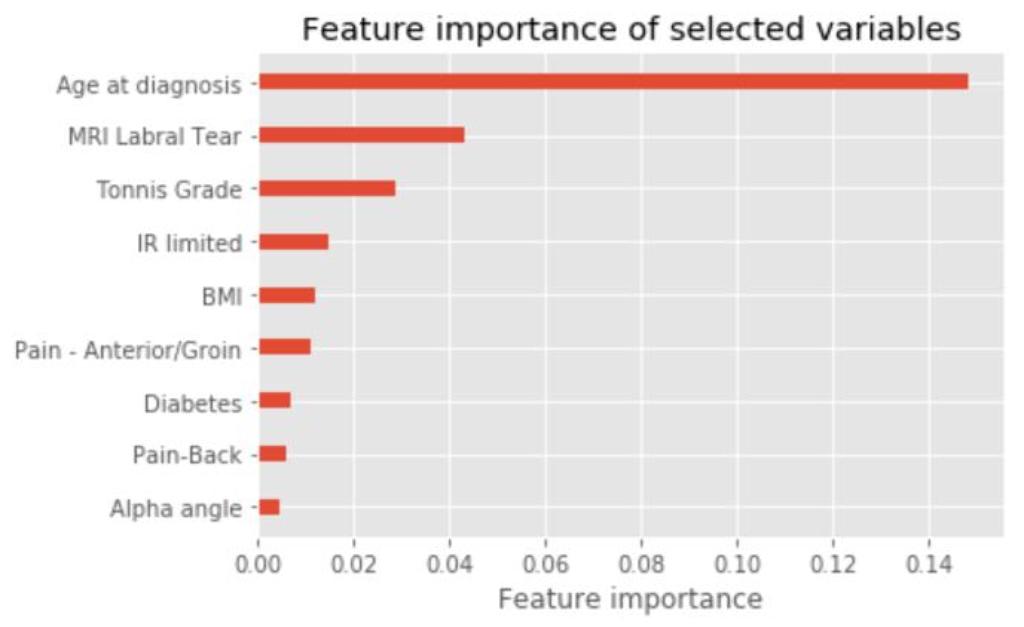
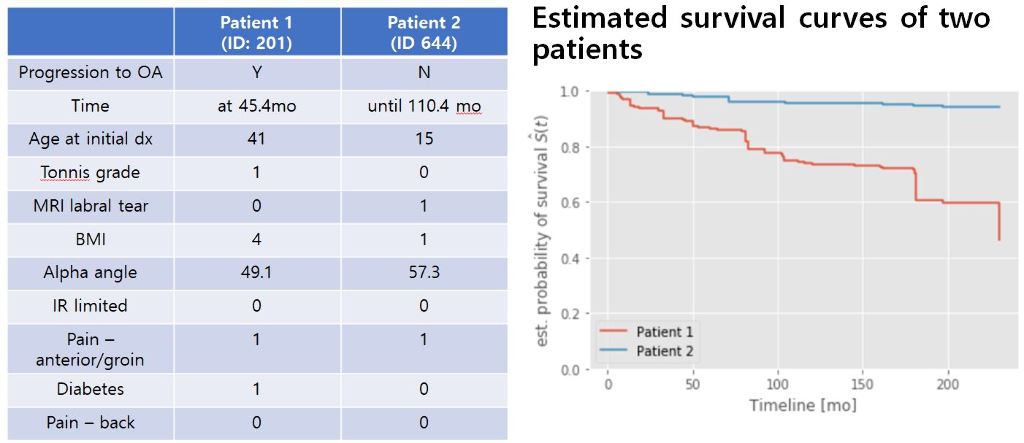
Of 1,012 patients, 90 (8.9%) progressed to OA over an average follow-up of 63.6 months. The average follow-up for non-OA patients is 95.4 months. There were no statistically significant survival differences between train and test set. Of the 37 variables, 9 variables were initially selected by univariate analysis. The selected features were – Age, Tonnis grade, MRI labral tear, Body mass index (BMI), alpha angle, limitation of internal rotation, anterior/groin pain, diabetes, and back pain. C-index of RSF model was 0.887 in train set and 0.845 in test set. While C-index of CPH model was 0.836 (train) and 0.840 (test). Figure 1 shows feature importance of RSF model. Survival curves for individual patients were created and tested for survival prediction in an online calculator (Figure 2).
Conclusion
With random survival forest model, individual survival curves can be assessed to discuss progression of hip osteoarthritis with patients. Age, MRI labral tear and Tonnis grade at initial presentation were most important three factors for osteoarthritis progression.
12.3.5 - Identifying Subscapularis Tendon Tears: Machine Learning Can Improve Diagnostic Accuracy
Abstract
Purpose
The purpose of this study was to use machine learning to develop a predictive model of subscapularis tears and delineate findings most helpful in identifying subscapularis tears preoperatively.
Methods and Materials
Between 2010 and 2020, 202 consecutive shoulders (57% male, mean age 58.8 years) underwent arthroscopic cuff repair by a single surgeon with particular attention to the arthroscopic diagnosis of subscapularis tears. Overall, 60% of patients had intraoperatively verified partial or full thickness tears of the subscapularis (50% of these were upper third). All radiographs and MRIs were reviewed independently in a blinded manner by two board-certified musculoskeletal radiologists. Patient demographics, physical exam, and imaging (tear, biceps status, fatty atrophy, and other) were included for model creation. An eXtreme Gradient Boosting (XGBoost) algorithm was selected due to its predictive power and efficiency. We used nested cross-validation to optimize hyperparameters with 10-fold validation.
Results
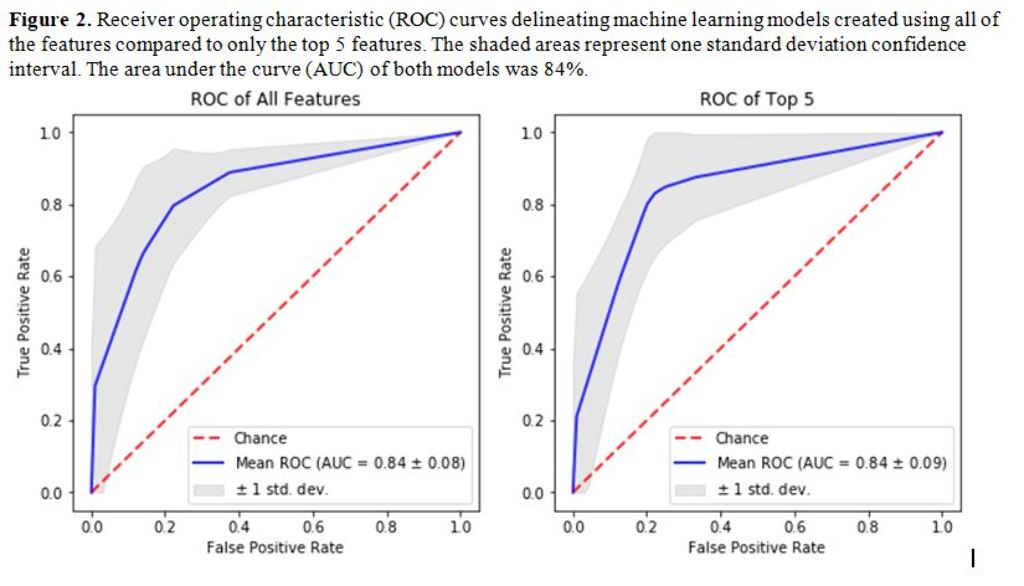
The first model was built using only imaging parameters and second model was built using imaging in addition to patient and physical exam parameters. The top five features included metrics related presence of tearing as evidenced on MRI (Figure 1). The overall area under the curve (AUC) of the model was 84.5% (Figure 2), which was deemed to be a very good model. The model’s accuracy did not increase with the addition of patient or physical exam parameters. In addition, isolating the model to only the top five features maintained the AUC of the model to 84%.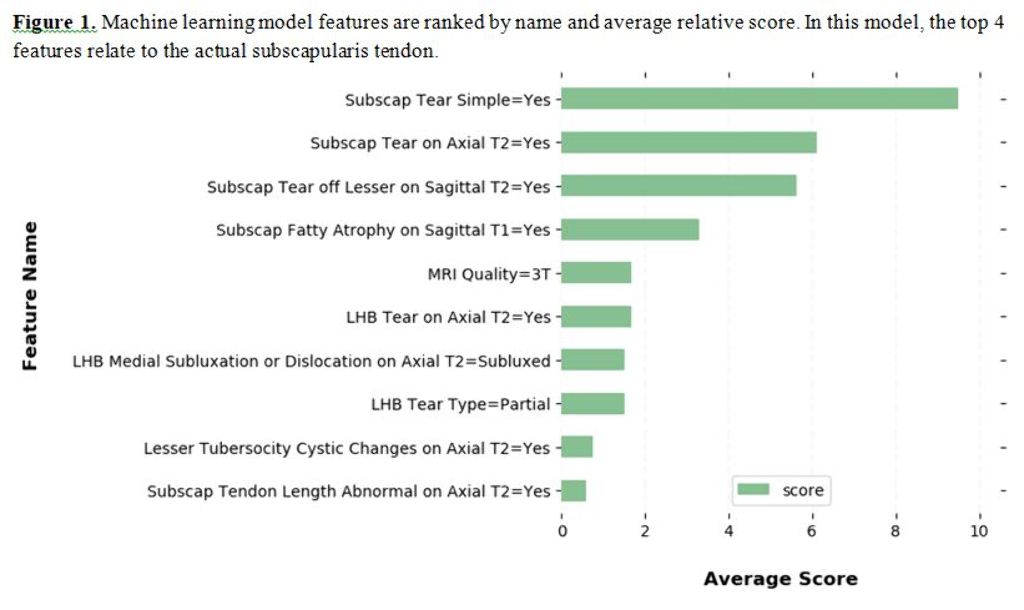
Conclusion
Machine learning was successful in predicting subscapularis tears in close to 85% of the patients and this accuracy did not decrease by isolating the model to the top features. The addition of physical exam or patient characteristics does not make a significant difference in the predictive ability of this particular model.
12.3.7 - Natural History of Femoroacetabular Impingement: Using Machine Learning to Evaluate Risk Factors For Osteoarthritis
Abstract
Purpose
The purpose of this study was to use machine learning to develop a predictive model of risk factors that influence progression to osteoarthritis (OA) in patients with FAI that did not have surgical intervention.
Methods and Materials
Between 2000 and 2016, medical records of all patients diagnosed with FAI in the Rochester Epidemiology Project (REP) were reviewed. Patient demographics, physical exam, and imaging characteristics (ex: cam lesion, alpha angle, Tonnis grade) were included for model creation. For the initial prediction method, a Gradient Boosting Machine algorithm was selected due to its predictive power and efficiency with 10-fold cross-validation. The primary outcome for progression was radiographic progression of symptomatic hip osteoarthritis via Tonnis Grade.
Results
1045 patients with a mean age 28.5 years, alpha angle of 61 degrees, Tonnis angle of 4.4 degrees were included. The mean follow-up was 24.9 years. A machine learning model was created using two steps. First model was built using only imaging parameters. Second model was build using both imaging parameters in addition to patient (age, BMI, etc) and physical exam (FAI impingement signs, groin pain, etc) parameters. The overall area under the curve (AUC) of the first model was 72.5% which was significantly improved to 81.9%. This model’s top two of the three features in order of importance were demographic related (age at diagnosis, BMI, Figure 1). The mean survival for the high-risk group was lower (121.9 months) than the low-risk group (201.9 months) for OA progression with survival of 90.4% vs 56.7% at 10-years (p<0.001).


Conclusion
In this long-term follow-up of a large geographic cohort treated nonoperatively, machine learning was successful in accurately predicting osteoarthritis progression given preoperative imaging, patient, and physical exam parameters. In addition, age, BMI, and Tonnis grade at initial presentation appear to be the most important three factors affecting osteoarthritis progression.



