12.3.1 - Fully Automated Deep Learning for Knee Alignment Assessment in Lower Extremity Radiographs: A Cross-Sectional Diagnostic Study
Abstract
Purpose
Accurate assessment of knee-alignment and leg-length-discrepancy is currently measured manually from standing-long-leg-radiographs (LLR), a process that is both time-consuming and poorly reproducible. The aim was to assess the performance of a commercial available AI-model, by comparing its outputs with manually performed measurements.
Methods and Materials
The AI-model was trained on over 15,000 radiographs to measure various clinical angles and lengths from LLRs. We performed a retrospective single-center analysis on 295 LLRs obtained between January 2015 and August 2020 from male and female patients over 18 years. AI-software and two orthopedists measured all LLRs. Kellgren-Lawrence score was assessed and reading time of each examination was automatically recorded. All measurements were compared and interchangeability, mean absolute deviation (sMAD) and intraclass-correlation (ICC) were calculated.
Results
A total of 295 LLRs from 284 patients (mean age, 65years (18; 90); 97 (34.2%) men) were analyzed. The AI-model produces outputs on 98.0% of the LLRs and had an accuracy of 89.2% when comparing the AI-outputs to the manually measured Ground-truth (100%). AI vs. mean observer revealed an sMAD between 0.39-2.19° for angles and 1.45-5.00mm for lengths. AI showed good reliability in all lengths and angles (ICC≥0.87) compared to mean observers. Non-inferiority comparing AI to the mean observer revealed an equivalence-index (γ) of 0.54° for the hip-knee-ankle-angle, 0.70mm for uncalibrated leg-length, and 6.70mm for calibrated leg-length. On average, AI was 130 seconds faster than clinicians.
Conclusion
Automated measurements of knee-alignment and length measurements produced with an AI tool result in reproducible, accurate measures with time savings compared to manually acquired measurements.
12.3.2 - Fully Automated Radiographic Measurements of The Pelvis
Abstract
Purpose
Pelvic radiographs help to evaluate geometry and morphometry of the hip joint. However, performing these measurements is not only a tedious, time-consuming task, but scientific literature also shows high inter- and intraobserver differences. Fully automated measurements could provide accurate, standardized and reproducible results more efficiently than the current radiological procedure.
Methods and Materials
AP pelvis radiographs of 62 patients (age: 36.9 ± 11.6 years; 34 female, 28 male) were included. Three orthopaedic surgeons independently performed the following measurements using an interactive planning software: Caput-collum-diaphyseal (CCD) angle, Lateral center-edge (LCE) angle, Tönnis angle, Sharp Angle and Extrusion index. The same images were also processed with a fully-automated, AI-based software (HIPPO, IBLab GmbH, Vienna). For hips with all three expert reads available (CCD: 119, LCE: 121, Other: 122), mean and standard deviation of the paired measurement differences was computed, comparing the averaged results of the expert readers (“mean-reader”) with HIPPO’s measurements as well as the expert readers against each other. An orthogonal linear regression was performed to assess proportional bias.
Results
Mean and standard deviation of the paired differences of “mean-reader” and HIPPO amounted to the following values (regression line slope in brackets): CCD: 0.22°±3.81° (1.03), LCE: -0.56°±2.99° (1.02), Tönnis: 1.52°±2.34° (0.94), Sharp: -0.92°±1.67° (0.97), Extrusion index: 2.08%±3.27% (1.14). Comparing “reader 1” and “reader 2” (most similar readers), yields the following: CCD: 0.58°±3.23° (0.91), LCE: -0.79°±2.16° (0.93), Tönnis: -0.93°±3.23° (1.19), Sharp: 0.76°±1.99° (1.00), Extrusion index: 0.22%±2.66% (0.91).
Conclusion
Regarding mean difference and regression line slopes, HIPPO’s performance is comparable to interobserver differences. Standard deviation shows increased variation of the paired differences, however, this is also true for inter-observer comparisons. These results indicate low absolute and proportional bias of HIPPO compared to expert readers. Automated radiographic analysis could therefore provide reproducible results for each AP pelvic image and help to identify radiographic signs of femoroacetabular impingement (FAI).
12.3.3 - Prospective Evaluation of Damage Marking Report Software to Predict Osteochondral Allograft Transplantation Graft Area
Abstract
Purpose
The purpose of this study was to evaluate the accuracy of the Damage Marking Report software (DMR) to correctly predict fresh osteochondral allograft (FOCA) graft area needed for surgery. Our hypothesis was the software would overestimate the area of the defect compared to the graft size used by a clinically acceptable amount.
Methods and Materials
Prospectively collected patient data was retrospectively identified from the two clinical sites. Inclusion criteria included patients 18 years and older who underwent FOCA to the distal femur. Exclusion criteria included defects of the trochlear and patella. MRIs were sent to the Joint Research Foundation for completion of the DMR (Figure 1).
We used nonparametric kernel-based regression to assess DMR variables. Trend curves are reported with 95% confidence bands. A linearized trend estimate was also calculated using Huber-biweight hybrid robust regression. We report the overall prediction performance (R2), regression weight (interpretable as the fraction of the predicted value that was actually used), and prediction accuracy (root-mean-square error).
Results
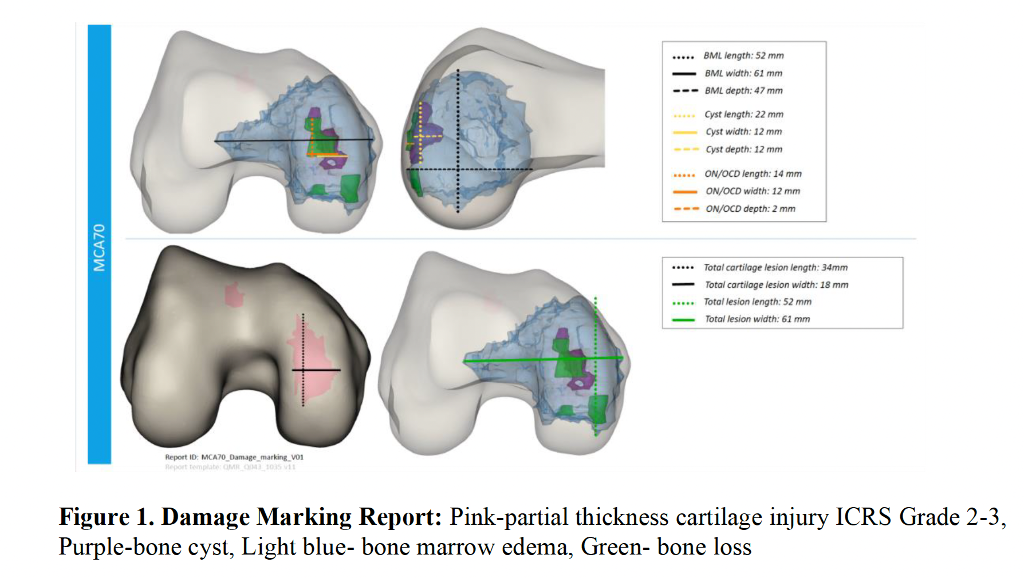
 A total of 36 FOCA surgeries were performed. The average graft size was 3.40 cm2 (range 1.13-7.07). The DMR overestimated the area of FOCA tissue in 30 subjects including 25 single FOCA grafts and 5 two-graft FOCAs. The DMR underestimated the area of FOCA tissue in 6 subjects including 5 single FOCA grafts and 1 two-graft FOCA. The overall DMR estimate of lesion size was larger than the area of graft used by roughly a factor of 8 (Figure 2).
A total of 36 FOCA surgeries were performed. The average graft size was 3.40 cm2 (range 1.13-7.07). The DMR overestimated the area of FOCA tissue in 30 subjects including 25 single FOCA grafts and 5 two-graft FOCAs. The DMR underestimated the area of FOCA tissue in 6 subjects including 5 single FOCA grafts and 1 two-graft FOCA. The overall DMR estimate of lesion size was larger than the area of graft used by roughly a factor of 8 (Figure 2).
Conclusion
The DMR overestimated the graft area used for the majority of FOCA surgeries including a range of graft area sizes and single and two-graft FOCA surgeries. These results suggest that the DMR modeling software can reliably overestimate the amount of graft needed for FOCA surgery. Reliably overestimating the amount of graft necessary may better refine the amount of allograft required for FOCA surgery.
12.3.4 - Patient-Specific Survival Prediction of Osteoarthritis in Hip Femoroacetabular Impingement Patients Using Machine Learning
Abstract
Purpose
The purpose of this study is (1) Predict survival curve of progression to OA for individual Hip FAI patient with machine learning algorithm and (2) compare performance of machine learning-based survival model and conventional Cox proportional hazard (CPH) model.
Methods and Materials
Between 2000 and 2016, all patients diagnosed with FAI in the Rochester Epidemiology Project were reviewed. Total of 1,012 patients with a mean age of 28.5 years were included. Demographics, physical exam, imaging features were included. The patient’s data was randomly split into Train (70%) and test (30%) sets.
Random survival forest (RSF), a non-parametric tree-based survival model is used to assess survival curves for individual patient. Concordance probability (C-index), the pairwise probability of lower patient risk given longer survival time, was used for evaluation.
Results
Of 1,012 patients, 90 (8.9%) progressed to OA over an average follow-up of 63.6 months. The average follow-up for non-OA patients is 95.4 months. There were no statistically significant survival differences between train and test set. Of the 37 variables, 9 variables were initially selected by univariate analysis. The selected features were – Age, Tonnis grade, MRI labral tear, Body mass index (BMI), alpha angle, limitation of internal rotation, anterior/groin pain, diabetes, and back pain. C-index of RSF model was 0.887 in train set and 0.845 in test set. While C-index of CPH model was 0.836 (train) and 0.840 (test). Figure 1 shows feature importance of RSF model. Survival curves for individual patients were created and tested for survival prediction in an online calculator (Figure 2).
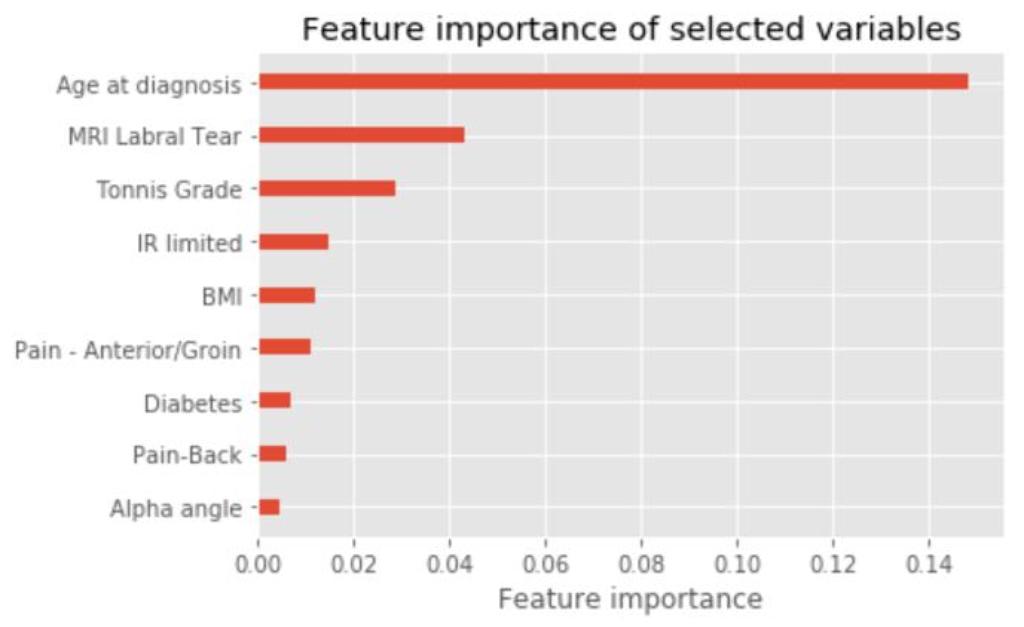
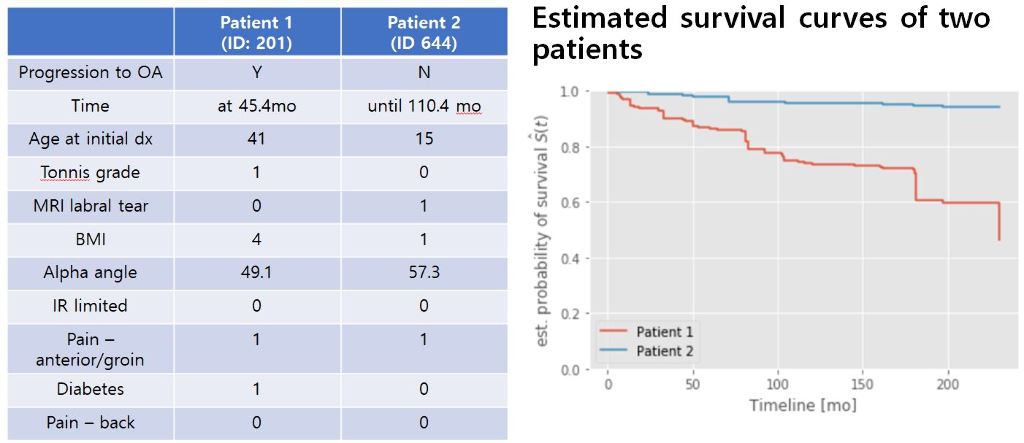
Conclusion
With random survival forest model, individual survival curves can be assessed to discuss progression of hip osteoarthritis with patients. Age, MRI labral tear and Tonnis grade at initial presentation were most important three factors for osteoarthritis progression.
12.3.5 - Identifying Subscapularis Tendon Tears: Machine Learning Can Improve Diagnostic Accuracy
Abstract
Purpose
The purpose of this study was to use machine learning to develop a predictive model of subscapularis tears and delineate findings most helpful in identifying subscapularis tears preoperatively.
Methods and Materials
Between 2010 and 2020, 202 consecutive shoulders (57% male, mean age 58.8 years) underwent arthroscopic cuff repair by a single surgeon with particular attention to the arthroscopic diagnosis of subscapularis tears. Overall, 60% of patients had intraoperatively verified partial or full thickness tears of the subscapularis (50% of these were upper third). All radiographs and MRIs were reviewed independently in a blinded manner by two board-certified musculoskeletal radiologists. Patient demographics, physical exam, and imaging (tear, biceps status, fatty atrophy, and other) were included for model creation. An eXtreme Gradient Boosting (XGBoost) algorithm was selected due to its predictive power and efficiency. We used nested cross-validation to optimize hyperparameters with 10-fold validation.
Results
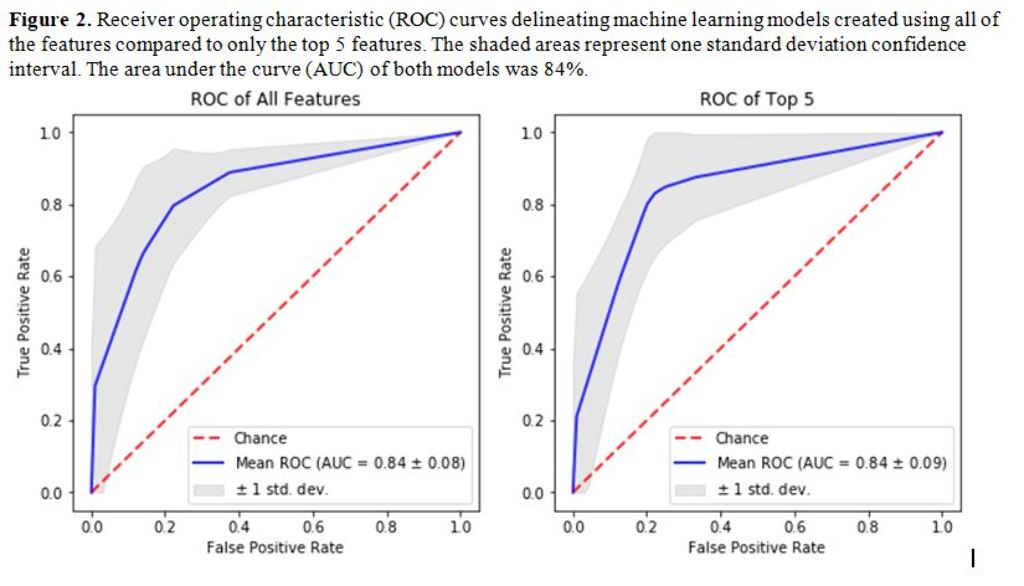
The first model was built using only imaging parameters and second model was built using imaging in addition to patient and physical exam parameters. The top five features included metrics related presence of tearing as evidenced on MRI (Figure 1). The overall area under the curve (AUC) of the model was 84.5% (Figure 2), which was deemed to be a very good model. The model’s accuracy did not increase with the addition of patient or physical exam parameters. In addition, isolating the model to only the top five features maintained the AUC of the model to 84%.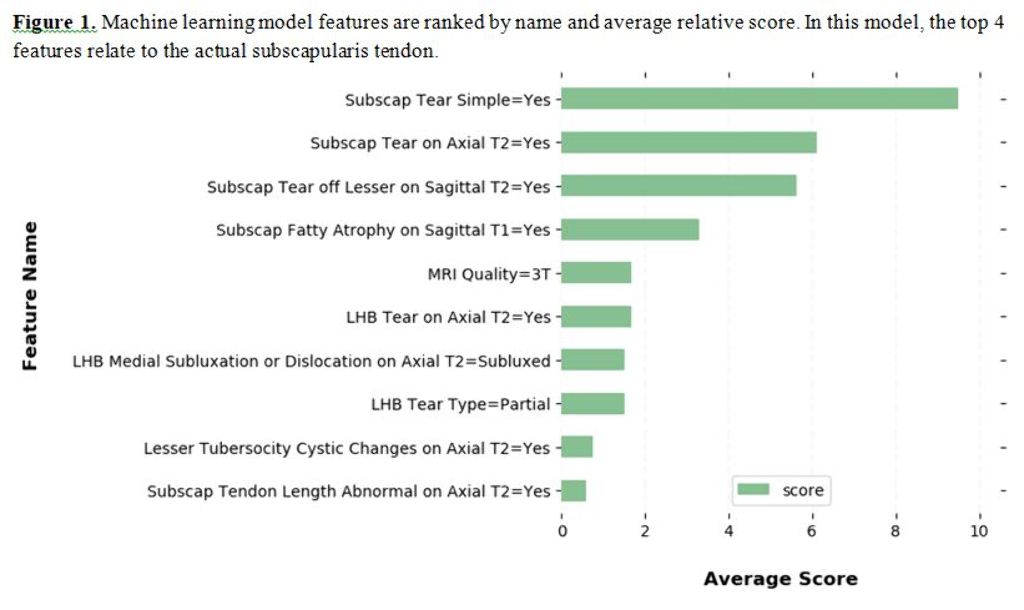
Conclusion
Machine learning was successful in predicting subscapularis tears in close to 85% of the patients and this accuracy did not decrease by isolating the model to the top features. The addition of physical exam or patient characteristics does not make a significant difference in the predictive ability of this particular model.
12.3.6 - Cost Utility Analysis of Arthroscopic Meniscal Repair on Collagen Matrix (AMMR) in Poland, Germany, United Kingdom and Switzerland
Abstract
Purpose
The objective of this study was to estimate the cost effectiveness of Arthroscopic Matrix-based Meniscus Repair (AMMR) in Poland, German, UK and Switzerland in the both the National Health Service (NHS) and from the perspective of private patients (PP).
Methods and Materials
A Markov health-state model was developed to evaluate the cost-utility analysis of AMMR compared to meniscectomy (ME) for patients with complex meniscus tear, using a 10-years horizon, modelling a cohort of 1000 patients. Initial probabilities and clinical course were simulated based on previously published data. A literature review identified different clinical outcome probabilities and health-related utility scores associated with each health state. Cost effectiveness was presented as an indicator of Incremental Cost-Utility Ratio (ICUR).
Results
In the 10 -year horizon, AMMR was associated with an increase in discounted quality-adjusted life-years (QALYs) to 7 778.25 as compared to 7 454.33 for ME. In both perspectives, (PNHS and PP) the ICUR cost is smaller than willingness to pay (WTP-125,955 PLN) parameter (PNHS-ICUR = 34,212.92 and PP-ICUR = 29,897.36) for Poland.
For Germany AMMR was associated with an increase in discounted QALYs to 7,858.64 as compared to 7,529.43 for ME. In both perspectives, (PNHS and PP) the ICUR cost is smaller than WTP (40,000 EUR) parameter (GNHS-ICUR = 10,661.75 and PP-ICUR = 22,924.05)
For UK, AMMR was associated with an increase in discounted QALYs to 7,844.55 as compared to 7,516.18 for ME. In both perspectives, (PNHS and PP) the ICUR cost is smaller than WTP (30,000 GBP) parameter (UKNHS-ICUR = 2,154.29 and PP-ICUR = 3,811.14).
For Switzerland, AMMR was associated with an increase in discounted QALYs to 8,073.35 as compared to 7,730.66 for ME. PP-ICUR (16,122.94) cost is smaller than WTP (100,000 CHF) parameter.
Conclusion
Despite the increase in costs, the procedure is cost-effective with standard thresholds used in all assessed countries for both analyzed perspectives
12.3.7 - Natural History of Femoroacetabular Impingement: Using Machine Learning to Evaluate Risk Factors For Osteoarthritis
Abstract
Purpose
The purpose of this study was to use machine learning to develop a predictive model of risk factors that influence progression to osteoarthritis (OA) in patients with FAI that did not have surgical intervention.
Methods and Materials
Between 2000 and 2016, medical records of all patients diagnosed with FAI in the Rochester Epidemiology Project (REP) were reviewed. Patient demographics, physical exam, and imaging characteristics (ex: cam lesion, alpha angle, Tonnis grade) were included for model creation. For the initial prediction method, a Gradient Boosting Machine algorithm was selected due to its predictive power and efficiency with 10-fold cross-validation. The primary outcome for progression was radiographic progression of symptomatic hip osteoarthritis via Tonnis Grade.
Results
1045 patients with a mean age 28.5 years, alpha angle of 61 degrees, Tonnis angle of 4.4 degrees were included. The mean follow-up was 24.9 years. A machine learning model was created using two steps. First model was built using only imaging parameters. Second model was build using both imaging parameters in addition to patient (age, BMI, etc) and physical exam (FAI impingement signs, groin pain, etc) parameters. The overall area under the curve (AUC) of the first model was 72.5% which was significantly improved to 81.9%. This model’s top two of the three features in order of importance were demographic related (age at diagnosis, BMI, Figure 1). The mean survival for the high-risk group was lower (121.9 months) than the low-risk group (201.9 months) for OA progression with survival of 90.4% vs 56.7% at 10-years (p<0.001).


Conclusion
In this long-term follow-up of a large geographic cohort treated nonoperatively, machine learning was successful in accurately predicting osteoarthritis progression given preoperative imaging, patient, and physical exam parameters. In addition, age, BMI, and Tonnis grade at initial presentation appear to be the most important three factors affecting osteoarthritis progression.
12.3.8 - Consensus Based Implementation Framework for New Treatments in Regular Care. A White Paper for Successful Implementation of ACI
Abstract
Purpose
Delay in access to new therapies, after completing the technical and clinical development program and approval by EMA and/or FDA, is undesirable, especially in areas of unmet medical need. Causes for such delays are national and/or regional reimbursement procedures prior to deciding on the implementation of new therapies in the national or regional health care system. Health authorities control the access of new therapies by requiring additional evaluations on top of the regulatory approval, such as evaluation of the added value and cost-effectiveness of the new therapy versus the available, often less expensive, standard of care. New therapies, therefore, have become budgetary competitors to current standard of care. Reimbursement procedures may differ largely per country and region in terms of extensiveness and complexity of reimbursement criteria, time needed and involved stakeholders necessary for decision making. Though physicians facilitated reimbursement procedures by providing consensus statements about the position of the new therapy in the treatment algorithm and therewith determining how ‘to treat the right patient with the right therapy’, this did not always result in a positive reimbursement decision.
Methods and Materials
To comply with the increased demand of health authorities and health insurers for control of the extent of the treated population and therewith budget control, we worked on a complementary approach called ‘a consensus-based implementation framework’ that facilitates the reimbursement and implementation process with minimal delays.
Results
This framework consists of a six-step approach covering assessment of added value, efficiency of the new therapy and its position in the treatment algorithm combined with determination of the organizational structure of the care in daily practice, establishing registries for outcomes and quality control measures.
Conclusion
This approach has been successful for implementation of autologous chondrocyte implantation for the knee in the Netherlands, which has an advanced reimbursement system, often serving as an example for other countries.
12.3.10 - Application of Deep Learning Models to Predict Achievement of PASS at Minimum 2-Year Follow-Up After Primary Hip Arthroscopy
Abstract
Purpose
To identify predictive factors for achieving PASS in patients undergoing primary hip arthroscopy and labral repair for femoroacetabular impingement syndrome (FAIS) and labral tears.
Methods and Materials
Data were prospectively collected and retrospectively reviewed on all patients undergoing primary hip arthroscopy and labral repair for femoroacetabular impingement syndrome (FAIS) and labral tears between July 2015 and May 2019. The primary outcome was achievement of PASS based on an anchor-question at minimum 2-year follow up. A Multilayer Perceptron Artificial Neural Network (MLP-ANN), Extreme Gradient Boosting (XGBoost), and logistic regression models were trained on an independent testing set of patients to identify significant predictors.
Results
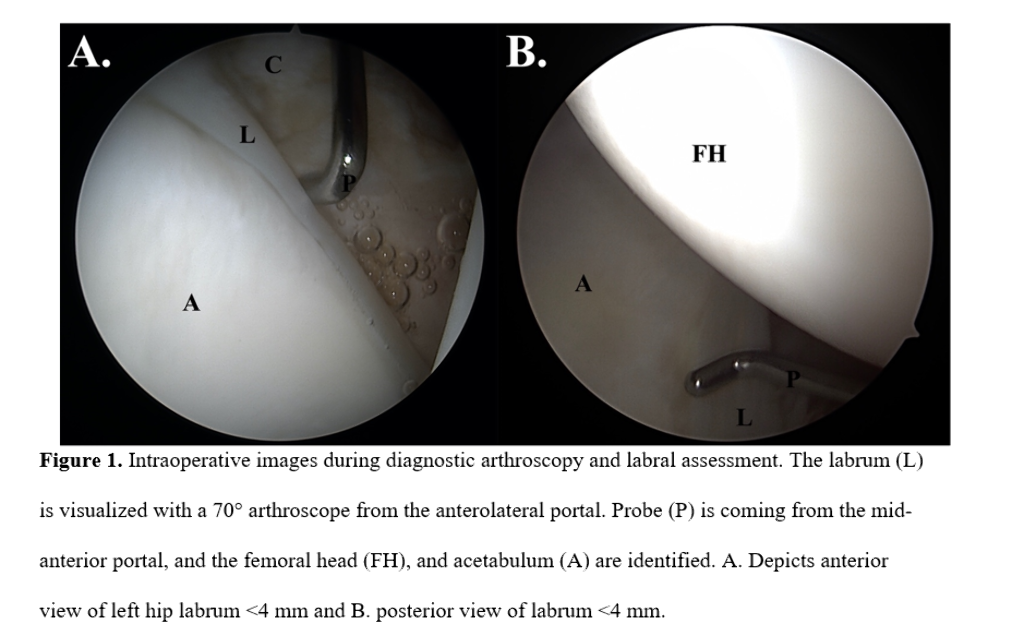
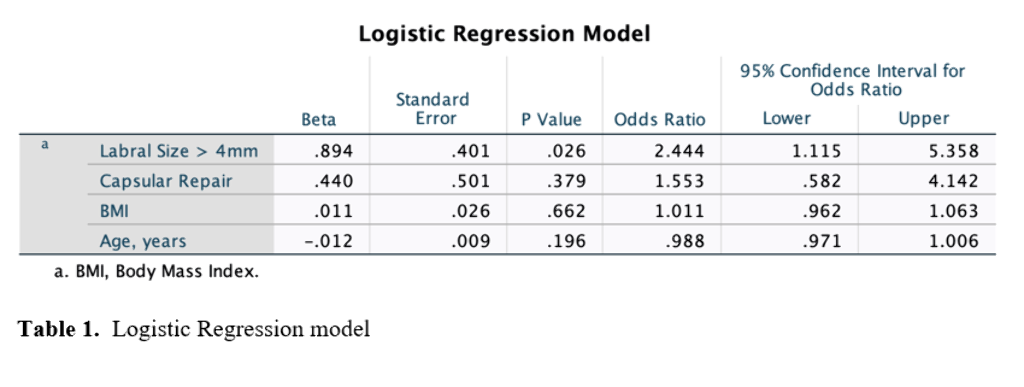
A total of 343 patients were included with 263/343 (76.7%) achieving the PASS threshold at minimum 2-year follow-up. A combination of 4 variables optimized model performance: capsular management (repair vs unrepair of interportal capsulotomy), labral size (<4 mm or ≥4 mm in the anterosuperior quadrant), age (years), and body mass index (BMI). The MLP-ANN model demonstrated the best accuracy (R2 = 78.1%) followed by the logistic regression (R2 = 71.8%) and XGBoost (R2 = 71.3%). The logistic regression found labral size ≥ 4mm to be the only statistically significant variable for predicting achievement of PASS (Odds Ratio: 2.444, P = 0.026). Patients with labral size ≥ 4mm achieved PASS at a rate of 78.7%, and patients with labral size < 4mm achieved PASS at a rate of 59.4% (P = 0.0244).
Conclusion
Labral size, capsular management, age, and BMI were found to be significant predictors of achieving PASS at minimum 2-year follow-up in patients undergoing primary hip arthroscopy and labral repair. Labral size ≥ 4 mm was the most statistically significant factor in favor of achieving PASS in this patient population.



