ICRS 2019 - Conference Calendar
23.2.1 - The Suitability Of Pre-Operative Magnetic Resonance Imaging In Predicting Accurate Cartilage Defect Sizes For Treatment With Cell Therapy
Abstract
Purpose
Clinicians are given guidance as to appropriate sizes of cartilage defects to treat with cell therapy. However, estimating the size on magnetic resonance imaging (MRI) may differ from ‘real-life’ areas. This study evaluates the accuracy of MRI to predict the size of articular cartilage lesions in the knee and compares against actual defect sizes recorded surgically.
Methods and Materials
This retrospective study included 64 patients (mean age 41.8±9.56 years), who underwent autologous cell implantation (ACI) performed by two different surgeons. Each patient received a pre-operative 3-T MRI at a mean of 6.1±3.0 weeks prior to cell implantation. MRIs were assessed by a single radiologist for the full-thickness defect measurement and the total abnormal defect area that they thought would be debrided. Defects were also measured by the surgeon pre- and post-debridement at arthrotomy at the cell implantation stage for comparison; post-debridement surgical measurements were used as the ‘gold standard’. Measurements were further assessed according to defect location (patella, trochlea, medial or lateral femoral condyle (MFC and LFC)).
Results
Ninety-two cartilage defects were analysed. Defects were significantly smaller pre-debridement (2.42±2.29cm2) than post-debridement (3.96±2.95cm2, p=0.0003). The MRI full-thickness defect size was significantly smaller than the pre-debridement size (1.18±1.9cm2 vs 2.42±2.29cm2 respectively, p=0.0001). In contrast, the MRI total abnormal defect area was not significantly different to the post-debridement defect size (3.11±2.78cm2 vs 3.96±2.95cm2), either when assessed collectively or by defect location. Whilst MRI still significantly underestimated pre-debridement defect sizes on the patella and MFC (p=0.024 and p=0.006, respectively), those on the LFC and trochlea were not significantly different.
Conclusion
These results indicate that measuring simply the full-thickness component of a cartilage defect on MRI will significantly underestimate the area to treat for ACI, but evaluating the whole abnormal area will better estimate the actual defect size for treatment. This is critical for surgical planning.
23.2.2 - The MOCART (Magnetic Resonance Imaging of Cartilage Repair Tissue) 2.0 Knee Score and Atlas
Abstract
Purpose
Since the first introduction of the MOCART score, a widely used semi-quantitative scoring system for the morphological assessment of cartilage repair tissue, significant progress has been made with both surgical treatment options as well as MR imaging of cartilage defects. Thus, the aim of this study was to introduce the MOCART 2.0 knee score — an incremental update on the original MOCART score — that incorporates this progression.
Methods and Materials
The degree of defect filling is assessed in 25% increments The severity of surface damage is determined in reference to cartilage repair length rather than depth. The signal intensity of the repair tissue is scored as minor abnormal or severely abnormal on PD TSE sequence only and considers hyperintense as well as hyointense repair tissue. The variables “subchondral lamina”, “adhesions” and “effusion” were removed and replaced by new variable “bony defect or bony overgrowth”. Four independent readers (two expert readers and two radiology residents) assessed 24 MRI examinations to define interrater and intrarater reliability using intraclass correlation coefficients (ICCs).
Results
The overall intra-rater (ICC = 0.88, p < 0.001) as well as the inter-rater (ICC = 0.84, p < 0.001) reliability of the expert readers was almost perfect. Based on the evaluation sheet of the MOCART 2.0 knee score, the overall inter-rater reliability of the inexperienced readers compared to expert reader 1 was moderate (ICC = 0.45, p < 0.01). With the additional use of the atlas, the overall inter-rater reliability of the inexperienced readers was substantial (ICC = 0.63, p < 0.001).
Conclusion
The MOCART 2.0 knee score was updated to account for important changes in the past decade and demonstrates almost-perfect inter- and intra-rater reliability in expert readers. In inexperienced readers use of the atlas may improve inter-rater reliability, and thus, increase the comparability of results across studies.
23.2.3 - Discrepancy between T2 mapping MRI and histological analyses for zonal composition of mesenchymal stem cell-based cartilage repair tissue
Abstract
Purpose
Quantitative magnetic resonance imaging (MRI) assessments such as T2 mapping have been recently studied to detect the biochemical composition and structure of articular cartilage. In the present study, we investigated the correlation of zonal image of T2 mapping MRI of the repair cartilage with the histology of biopsy specimen at the corresponding area in five patients who underwent the implantation of a scaffold-free tissue-engineered construct (TEC) generated from autologous synovial mesenchymal stem cells (MSCs) to an isolated cartilage lesions, and aim to elucidate the efficacy and limitation of T2 mapping MRI for the evaluation of cartilage repair.
Methods and Materials
We performed both T2 mapping MRI and histological evaluation of biopsy specimen at the identical area in all patients at 48 weeks postoperatively, and T2 values and histological scores were compared at superficial, middle and deep zone of repair tissue.
Results
Histology showed that the repair tissue in the superficial zone was dominated by fibrous tissue and the ratio of hyaline-like matrix increased with the depth of the repair tissue, leading to the dominance by hyaline cartilage–like tissue in the deep zone (Figure 1). There was significant difference between superficial and middle/deep zones in histological scores. Conversely, there was no statistical significances in T2 value detected among zones (Figure 2). Accordingly, there were no correlations detected between histological scores and T2 values in each zone.

Conclusion
Such discrepancy of the data between T2 mapping and histology suggests that T2 mapping failed in detecting the collagen architecture and composition of repair cartilage. This suggests that the resolution of current quantitative MRI might not be enough to depict the difference in zonal collagen architecture in repair cartilage. Furthermore, although invasive, histologic assessment is likely still more reliable method for evaluation of tissue quality.
23.2.4 - The development of a magnetic resonance scoring system for evaluating osteochondral healing in preclinical models – the 'AMOS’ score.
Abstract
Purpose
The purpose of this study was to create and assess the reliability of an Animal Magnetic resonance imaging Osteochondral Score (AMOS) to evaluate the healing of experimentally created osteochondral defects in preclinical models.
Methods and Materials
The AMOS score consists of an objective score and four subjective scores (integration, repair tissue surface, infill signal intensity and signal change outside surgical site). The AMOS score was applied to lesions in forty-six sheep using an ovine medial femoral condyle osteochondral defect model as an exemplar. These defects were subsequently evaluated histologically using the modified O’Driscoll score.
Results
The AMOS scores recorded ranged from 35 to 100. The AMOS score had 92.5% inter-rater reliability and 80% intra-rater reliability for the four subjective components. The mean inter-rater-reliability was 85% (+/- >1%) for integration; for intensity of infill, the mean inter-rater reliability was 95% (+/- 0%); the mean intra-reliability was 92.5% (+/- 2.5%) for repair tissue surface; and the mean inter-rater reliability was 97.5% (+/- 2.5%) for signal change outside the operated site. No correlation was found between the AMOS score and the modified O’Driscoll score.
Conclusion
The AMOS score had high inter-rater reliabilities, suggesting that it would be an effective scoring system. The AMOS score is a user-friendly semi-quantitative method of assessing osteochondral defect from magnetic resonance appearance for following ovine defect changes. The lack of correlation between AMOS and histological scorings reflects their different sensitivities to healing, suggesting that the AMOS score is complementary to histological evaluation.
23.2.5 - Elliptical, Stacked, and Single Osteochondral Allograft Transplantation for Large Knee Chondral Defects: One-Year MRI Outcomes
Abstract
Purpose
Osteochondral allograft transplantation (OCA) is a proven cartilage restoration procedure for patients with large chondral defects. However, elongated condylar lesions pose a challenge for dowel OCA in restoring articular surface congruity. Recently, instrumentation to harvest a single, elliptical allograft (BioUni, Arthrex) has been developed for treating ovoid lesions without requiring an adjacent-plug (stacked or snowman) technique (Figure 1). The purpose of this study was to compare 1-year MRI outcomes of patients treated with elliptical, stacked, or single OCA using the Osteochondral Allograft MRI Scoring System (OCAMRISS) and percent osseous integration.

Methods and Materials
A retrospective review on patients treated from 2000 to 2018 with OCA for condylar defects of the knee was conducted. Inclusion criteria included those followed prospectively with a MRI at ~1 year after surgery. OCAMRISS and osseous integration scores (0-25%; 26-50%; 51-75%; 76%-100%) were graded by a musculoskeletal radiologist blinded to the outcomes. Comparisons of demographics and MRI scores were performed with the ANOVA.
Results
A total of 48 knees (mean age, 35.8 years; 70% male) met the inclusion criteria and were treated with either elliptical (n=19), stacked (n=19), or single (n=19) OCA. Mean time to post-operative MRI was 10.7, 11.1, and 12.4 months, respectively (p=0.17). There were no significant differences in demographics or number of prior ipsilateral knee surgeries among groups. Bone, cartilage, ancillary, and total OCAMRISS scores were not significantly different between groups (Table 1). A trend towards a higher percentage of osseous integration (single>stacked>elliptical) was noted which correlated with less transplanted allograft bone, however, these differences were not significant (p=0.15).

Conclusion
One-year OCAMRISS and osseous integration scores did not differ among patients treated with elliptical, stacked, or single OCA. Further investigation is needed to explore potential differences in clinical outcomes and long-term osseous integration between elliptical and stacked OCA for the treatment of elongated condylar defects of the knee.
23.2.6 - Automated detection of Bone Marrow Edemas from MRI: data from the Osteoarthritis Initiative
Abstract
Purpose
Bone marrow edemas (BMEs) are defined as localized build-up of fluids within the bone marrow, often leading to swelling, which are strongly associated with pain and progression of joint deterioration. However, manual reading of BMEs is a time-consuming task for the physician. Here, we ask if a deep neural network can automatically detect the presence or absence of BME from T2 sequences of Magnetic Resonance images.
Methods and Materials
We collected 24.885 MRI sequences from the OAI study with associated labels of 10.429 for BMEs in the form of MOAKS scores. Sequences were classified for the presence of BMEs if the total number of BMEs exceeded 1 and its reported size of less than 33% in the respective compartment. This dataset was split into training/testing datasets of sizes 773 and 465, respectively. A deep neural network was trained on 1083 training/validation splits of the training dataset. Training performance was assessed by classification accuracy and testing performance was assessed by the area under the ROC curve (AUC).
Results
The final training accuracy on the training/validation datasets was 1 and 0.81. We find that our deep neural network achieves an AUC of 0.90 on the testing dataset at the detection of BMEs from T2 MRI sequences. Furthermore, saliency analysis reveals the location of these BMEs.
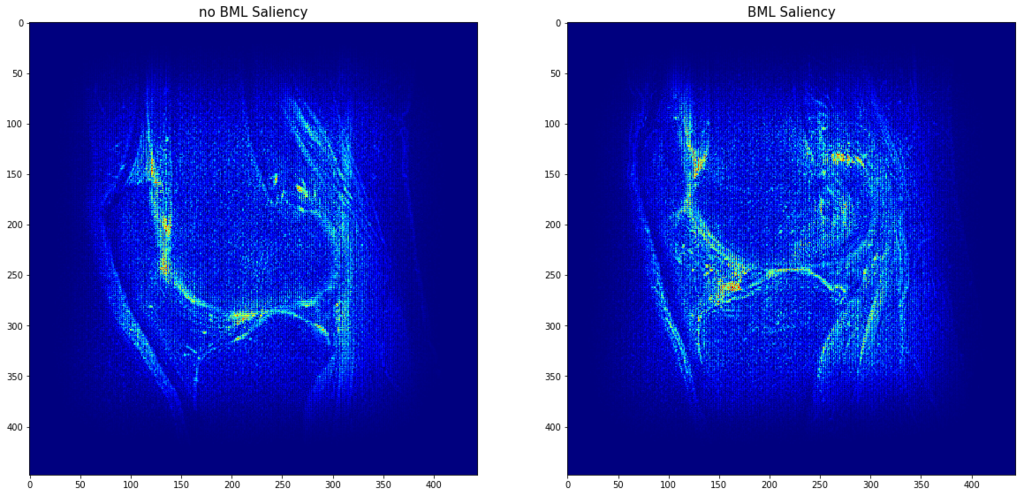
Conclusion
Our results show that our method performs excellently at detecting BMEs from MRI. This automated method assesses a full MRI sequence under 2 seconds and, combined with automatic highlighting of the detected BMEs, can substantially decrease physicians’ time spent on this routine task.
23.2.7 - Cationic contrast enhanced computed tomography characterizes articular cartilage in an equine impact model
Abstract
Purpose
Current imaging methods are unable to detect subtle articular cartilage injury. Loss of glycosaminoglycans (GAGs) is a hallmark of early osteoarthritis. Cationic contrast enhanced computed tomography (CCECT) is a new diagnostic method capable of predicting GAG content and the compressive strength of normal cartilage, but its capacity to distinguish normal from early degenerative cartilage is unknown. The objectives of this study are to induce subtle articular cartilage injury in vivo and use CCECT to distinguish normal from degenerative cartilage. We hypothesize that CCECT attenuation of articular cartilage will correlate with its biochemical, mechanical and histological properties.
Methods and Materials
Mechanical impact injury (41 MPa, 32.7 mm2) was applied to the equine femoral trochlear surface in vivo to establish subtle cartilage degeneration using horse-matched and site-matched controls. CCECT was performed in vivo (clinical) and postmortem (microCT). Articular cartilage was characterized by glycosaminoglycan (GAG) content, biochemical moduli and histological scores. Subchondral bone beneath each cartilage site was characterized by volume density (BV/TV) and trabecular number (Tb.N.), thickness (Tb.Th.) and spacing (Tb.Sp.).
Results
CCECT attenuation (microCT) of cartilage correlated with GAG (r=0.74, P<0.0001), equilibrium compressive modulus (Eeq)(r=0.79, P<0.0001) and safranin-O histological score (r=-0.66, P<0.0001) of cartilage (Figure 1), and correlated with BV/TV (r=0.37, P=0.0005), Tb.N. (r=0.39, P=0.0003), Tb.Th. (r=0.28, P=0.0095) and Tb.Sp. (r=-0.44, P<0.0001) of bone. Mean [95% CI] CCECT attenuation at the impact site (2215 [1987, 2443] Hounsfield Units [HUs]) was lower than site-matched controls (2836 [2490, 3182] HUs, P=0.036) and corresponded with safranin-O stain distribution (Figure 2). Clinical cationic CECT attenuation correlated with GAG (r=0.23, P=0.049), Eeq (r=0.26, P=0.025) and safranin-O histology score (r=-0.32, P=0.0046).


Conclusion
Cationic CECT (microCT) reflects biochemical, mechanical and histological articular cartilage properties enabling segregation of subtly degenerated from healthy tissue. CCECT also reflects bone morphometric properties on CT. Cationic CECT is capable of characterizing articular cartilage properties in clinical scanners.
23.2.8 - Anterior tibiotalar fat pad morphology and signal intensity on MRI are correlated with patient characteristics and joint pathology
Abstract
Purpose
In this study, we tried to investigate the innovative concept of the ATFP as missing link in the pathogenesis of persistent complaints after ankle sprain and potential source driving inflammation in the development of ankle osteoarthritis.
Methods and Materials
The present study is a secondary analysis of an observational case control study by Van Ochten et al. We included 106 patients with a Kellgren & Lawrence score of 0 in the tibiotalar joint on x-ray. T1 MRI scans were assessed for the signal intensity and area of the ATFP by mapping the fat pad in ‘Mimics 18.0’. After importing those mapped scans in the program ‘MATHLAB’, quantitative values of intensity and area were generated. Those values were statistically tested for correlations with patient characteristics and structural abnormalities by univariate and multivariate linear regression.
Results
MRI signal intensity of the ATFP is associated with BMI (p= 0.03), sex (p<0.01) and age (p= 0.01). ATFP area is correlated with sex (p<0.01) and presence of pre-OA signs in the subtalar joint (p= 0.01). After multivariate analysis, correcting for sex, subtalar pre-OA signs and BMI, persistent complaints were associated with ATFP area (p= 0.04).
Conclusion
This study demonstrates the involvement of the ATFP in hindfoot joint pathology. ATFP MRI characteristics were also influenced by patient characteristics. Further research should confirm these findings in a more elaborate population including OA patients, focus on histological validation and determine underlying pathogenic processes that may explain the observed correlations.
23.2.9 - Computed tomography parameters following osteochondral allograft transplantation do not correlate with patient reported outcomes
Abstract
Purpose
Prior studies have shown favorable and durable clinical outcomes following osteochondral allograft (OCA) transplantation to treat osteochondral defects; however, there is not an established imaging modality to evaluate tissue healing relative to clinical outcomes. The purpose of this study was to define parameters for OCA bone healing using computed tomography (CT) and to assess for correlation with patient reported outcomes (PROs).
Methods and Materials
CT scans were obtained 5.8 ± 1.9 months post-operatively for 60 patients who underwent OCA transplantation for articular cartilage defects of the knee. CT parameters (Figure 1) were summarized for each patient relative to the cohort using Mahalanobis distances, which were further assessed for covariation with demographic and surgical variables. Patient reported outcomes were collected pre-operatively and at post-operative intervals. Structural equation modeling (SEM) was employed to assess for correlation of CT parameters with PROs closest in time to CT, and with PRO change from pre-operative baseline to final follow-up, adjusted for duration.

Results
When scaled by covariance among CT parameters, the collection of CT scans was distributed according to multivariate normality and without outliers. Variance in CT parameters was independent of age, gender, BMI, prior surgery, number of grafts, lesion size, and location. No significant correlation (p>0.12 across all comparisons) was identified in any combination of CT parameter and most proximal PRO or change in PRO (Table 1). There was, however, a uniformly positive association between host bone density and change in PRO, independent of demographic and surgical factors.

Conclusion
Computed tomography has potential to measure tissue-level changes following OCA transplantation. The identified CT parameters were normally distributed within the study population and may be useful in evaluating bone healing and incorporation in individual patients. These metrics collected from a single post-operative CT scan, however, do not correlate with clinical outcomes at 6-months or longitudinal follow-up.
23.2.10 - Apparent Density of osteoarthritic cartilage is influenced by integrity of the superficial zone in non-equilibrium contrast-enhanced CT
Abstract
Purpose
Investigate the feasibility of using non-equilibrium contrast-enhanced computerized tomography (CE-CT) to address the problem of staging cartilage injury and osteoarthritis (OA) in species with thin cartilage.
Methods and Materials
A pilot study was performed on n=39 bovine osteochondral blocks with three types of superficial cartilage damage: intact, fibrillated and delaminated. Samples were exposed to 60% CystoConray or lactated ringer’s (LRS) solution for 10 minutes, then imaged at a resolution of 45 microns. In the in-vivo study OA was induced by arthroscopic meniscal destabilization (MMT) in n=20 adult female sheep plus n=4 as naive controls. One intra-articular injection of anionic media was given 13 weeks post-MMT and CT images of both stifles joints were obtained 10 minutes after injection. Sheep were sacrificed at two time points: 3 months post-MMT (early OA (n=9)), or 12 months (late OA n = 11) and the normal controls. Stifles were dissected and the proximal tibia was immersed in contrast media for 10 minutes prior to micro CT. Cartilage samples were harvested for a proteoglycan biochemical assay along with osteochondral sections for histology.
Results
Removal of the superficial cartilage zone resulted in elevated apparent density of bovine cartilage compared to intact controls (p<0.01). Cartilage visibility in the stifle of anesthetized sheep was also significantly improved during CT imaging by the contrast after a 10 minute delay (p<0.05) compared to the non-contrast enhanced contralateral stifle. Apparent density in ex vivo cartilage correlated negatively (r = -0.56) with sGAG in the medial tibial plateau (R2 = 0.28, p<0.001). OARSI scoring for collagen pathology differed significantly (p<0.05) between early and late OA groups and correlated positively (r = 0.41, p<0.05) with apparent density.


Conclusion
While changes in proteoglycan levels partially explain variance in apparent density, degree of superficial zone loss influences the uptake when using a short-term exposure time to evaluate cartilage and OA progression.



