Welcome to the ESPNIC Xperience Programme Scheduling
The meeting will run on Central European Summer Time
NASOTRACHEAL VERSUS OROTRACHEAL INTUBATION AND POST EXTUBATION AIRWAY OBSTRUCTION IN CRITICALLY ILL CHILDREN: AN OPEN-LABEL RANDOMIZED CONTROLLED TRIAL
Abstract
Background and Aims
The data on long-term nasotracheal intubation among mechanically ventilated critically ill children and its effect on post-extubation airway obstruction (PEAO) is limited
To compare the rate of PEAO with nasotracheal and orotracheal intubation
Methods
This open-label randomized controlled trial was conducted in PICU of a tertiary care and teaching hospital in North India from January-December 2020 involving intubated children aged 3 months-12 years. After written informed consent, children were randomized into orotracheal or nasotracheal groups. Children in orotracheal group were continued with same treatment whereas children in nasotracheal group were re-intubated through the nasal route. Post-extubation, modified Westley’s croup score (mWCS) was used at different timed points to monitor for PEAO. The primary outcome was the rate of PEAO and secondary outcomes were time taken for intubation, number of intubation attempts, complications during intubation, accidental extubation, repeated intubations, tube malposition/displacement, endotracheal tube blockade, ventilator associated pneumonia, skin trauma, extubation failure, duration of PICU stay, and survival
Results
seventy children were randomized into nasotracheal (n=30) and orotracheal (n=40) groups. Both the groups were similar in baseline characteristics, diagnosis, and severity scores. The rates of PEAO were lower in nasotracheal group than orotracheal groups (10% vs. 20%, p=0.14), although the difference was not statistically significant. Among secondary outcomes, the time taken for intubation was significantly longer (85 second vs. 48 seconds, p<0.001) in nasotracheal group and other secondary outcomes were similar in two groups
Conclusions
PEAO was lower with nasotracheal intubation than orotracheal intubation, although the difference was not statistically significant
COMPARISON BETWEEN EARLY INTUBATION AND BAG-VALVE-MASK VENTILATION AND TIDAL VOLUME GUIDED VENTILATION VERSUS STANDARD VENTILATION IN A PEDIATRIC ANIMAL MODEL OF CARDIOPULMONARY RESUSCITATION.
Abstract
Background and Aims
To compare early intubation vs bag-valve-mask ventilation (BVMV), and expiratory tidal volume (Vte) real-time guide ventilation vs standard ventilation (non-guidance ventilation) in a pediatric animal model of asphyxial cardiac arrest (CA).
Methods
Piglets were randomized into five groups: 1: intubated and Vte-guided ventilation (10 ml/kg); 2: intubated and standard ventilation (SV); 3: BVMV and Vte-guided ventilation (10 ml/kg); 4: BVMV and standard ventilation; 5: intubated and Vte-guided ventilation (7 ml/kg). To give 30 breaths-per-minute a metronome was used. Return of spontaneous circulation (ROSC) were compared between groups. A linear mixed model was performed to analysed EtCO2 (end tidal CO2), VCO2 (CO2 output), MAP (mean arterial pressure), DAP (diastolic arterial pressure) and VTe during resuscitation.
Results
Seventy-nine piglets weighing 11.3±1.2 kg were included. Twenty-six (32.9%) achieved ROSC (group 1: 41.2%; group 2: 40.0%; group 3: 23.5%; group 4: 20% and group 5: 40%). Survival rate was higher in intubated piglets (40.4%) than BVMV (21.9%), p=0.08. No differences in ROSC were found between VTe-guided (30%) and SV (34.7%) p=0.67). ROSC animals, presented higher EtCO2, VCO2, MAP and DAP during resuscitation, than non-survivors (p<0.01) (figure 1). Intubated animals compared to BVMV presented higher EtCO2, VCO2 and Vte (p<0.04) throughout resuscitation (figure 1). Vte were lower in Vte-guided group than in SV (p<0.01).

Figure 1 Linear mixed model
Conclusions
In an animal model of pediatric CA, early intubation obtained higher non-significant survival rates. Vte was higher in intubated animals and with SV. Better ETCO2, VCO2, MAP and DAP were achieved in ROSC animals.
SEPTIC SHOCK MANAGEMENT GUIDED BY ULTRASOUND: A RANDOMIZED CONTROLLED PILOT TRIAL (SEPTICUS TRIAL)
Abstract
Background and Aims
Current fluid bolus therapy (FBT) practice increases risk of fluid overload and mortality. Ultrasound-guided Septic Shock Management (USSM) is a proposed protocol, which is assess fluid responsiveness, stroke volume index (SVI), cardiac index (CI), and systemic vascular resistance index (SVRI) by ultrasound cardiac output monitor (USCOM). We aim to determine the difference outcomes between USSM and American College of Critical Care Medicine (ACCM)protocol, i.e.: 72-hour mortality rate, CI, SVI, SVRI, lung ultrasound score (LUSS), and incidence of hepatomegaly.
Methods
It was single center, open-label randomized-controlled pilot trial. Subject was randomized into intervention (USSM) and control (ACCM) group. All subjects received FBT 10-20 mL/kg and performed USCOM measurement as initial step. In intervention group, clinical and hemodynamic (USCOM) parameters were assessed to guide treatment. Whereas only clinical parameter was assessed in control group. FBT was terminated either if therapeutic goals achieved or fluid-refractory occurred (SVI or CI did not increase >10% in intervention group, and hepatomegaly or rales occurred in control group). Outcomes, except mortality, was evaluated at 1 hour. The study was approved by the ethical committee of Universitas Brawijaya.
Results
Thirty six subjects were enrolled. Total fluid was 26.1 (SD 8.5) and 29.4 (SD 11.1) mL/kg in intervention and control group, respectively. There were higher 72-hours mortality rate (p=0.009), LUS score (p<0.001), and hepatomegaly incidence (p<0.001) in control group. SVI, CI, and SVRI did not differ significantly.
Conclusions
USSM protocol could prevent 72-hours mortality and reduce the incidence of tissue edema.
A HYBRID FORM OF TELEMEDICINE AND QUALITY IMPROVEMENT: A UNIQUE WAY TO EXTEND INTENSIVE CARE SERVICES TO NEONATES IN MEDICALLY UNDERSERVED AREAS
Abstract
Background and Aims
To assess the treatment outcomes of all babies managed by the hybrid telemedicine system in extremist affected Sick
newborn care unit (SNCU) at Dantewada compared with conventional management provided to a medically similar
population in SNCU Bijapur, Chhatisgarh, India.
Methods
This prospective noninferiority study was done at SNCU Dantewada and Bijapur starting from July 2018 to December 2020. All infants admitted in these SNCUs were included. Control group included babies admitted in SNCU Bijapur without tele-supervision. Infants requiring advanced subspecialty services were excluded. The Skype technology was used for tele-rounds.The nurse in the SNCU contacted the PI by a phonecall to initiate daily rounds by telemedicine. The one-day visit by PI per month included initiation of QI projects and hand holding. Patient outcome measures, including length of stay, type and duration of respiratory support, length of antibiotic therapy, and time to full enteral feedings was collected.
Results
598 and 516 neonates at Dantewada and Bijapur were included respectively. Prematurity, RDS, TTNB and hypoglycemia were the top four diagnosis at both centers. Neonates at Dantewada had less mortality (p=0.032), shorter hospital stays 3.1days (95% CI 0.46,34.8), reached full enteral feeds sooner 1.8 days (95% CI 0.03,13.64), fewer days of supplemental oxygen 2.15 days (95% CI 0.48,19.07), and fewer days on noninvasive support 1.76 days (95%CI 0.79,8.78). Antibiotics use beyond 48 h was lesser in Dantewada patients (8% vs. 32%).
Conclusions
Hybrid telemedicine is a safe and effective strategy that may be used in extending intensive care to sick neonates in resource limited areas.
A SYSTEMATIC REVIEW AND POOLED PREVALENCE OF PAEDIATRIC DELIRIUM IN CRITICALLY ILL CHILDREN
Abstract
Background and Aims
Paediatric Delirium (PD) is a neuropsychiatric complication that occurs during the management of children in the PICU/NICU. Delirium can be classified as hypoactive (decreased responsiveness and withdrawal), hyperactive (agitation and restlessness), and mixed.
PD has historically been underdiagnosed or misdiagnosed. An estimation of the pooled prevalence of PD using validated assessment tools, and identification of risk factors will help improve recognition and drive prevention and management.
Methods
A systematic search of PubMed, EMBASE and CINAHL was undertaken for eligible articles that estimated a prevalence of PD in the PICU/NICU. Data was extracted, quality assessed and a pooled prevalence calculated.
Results
Thirty-one observational studies describing PD prevalence ranging from 7-66% were included. Hypoactive delirium was the most prevalent sub-type, with a pooled prevalence of 34% (95%CI 27,41) estimated from 17 studies that used the CAPD score. Risk factors identified included; younger ages, sicker patients, use of restraints, number and cumulative dose of benzodiazepines and opioids. PD was associated with longer durations of mechanical ventilation, stays and increased costs. Data on mortality association are limited and conflicting.

Conclusions
PD affects one third of critical care admissions and is resource intense. Routine assessment in clinical practice may facilitate earlier detection and management strategies. Modifiable risk factors can be classified as patient, pharmacotherapy or clinical care related. Early mobility and lessening use of contributing factors may reduce PD occurrence. Longitudinal prospective multi-institutional studies to further investigate the presentations of the different delirium subtypes and modifiable risk factors that potentially contribute to the development of PD, are required.
PREDICTION OF PEWS AT PICU; THE USE OF A NEW MACHINE LEARNING METHOD
Abstract
Background and Aims
The increasing amounts of data pose a great demand on ICU staff because of data overload. Medical decision making is a difficult and labor-intensive process, especially with multiple, continuous streams of vital sign data. Machine learning (ML) may be used to support decision making by facilitating the recognition of clinical patterns in this data.
Methods
This single-center, retrospective, cohort study included 1208 patients admitted to the PICU of the University Medical Center Utrecht, The Netherlands. Six streams of recorded vital signs (Figure1) were collected from the EMR, resulting in a set of 1,5 million data time points. The ML method uses Symbolic Aggregate approXimation (SAX) to summarize the streams of vital signs leading up to and including the current time point. The patient of interest is then matched with historic patients based on those SAX patterns. The disease courses of the matched patients are aggregated into a predicted disease course for each vital sign. To get a summary of predictive performance across multiple variables, the vital signs are combined into a Pediatric Early Warning Score (PEWS).
Results
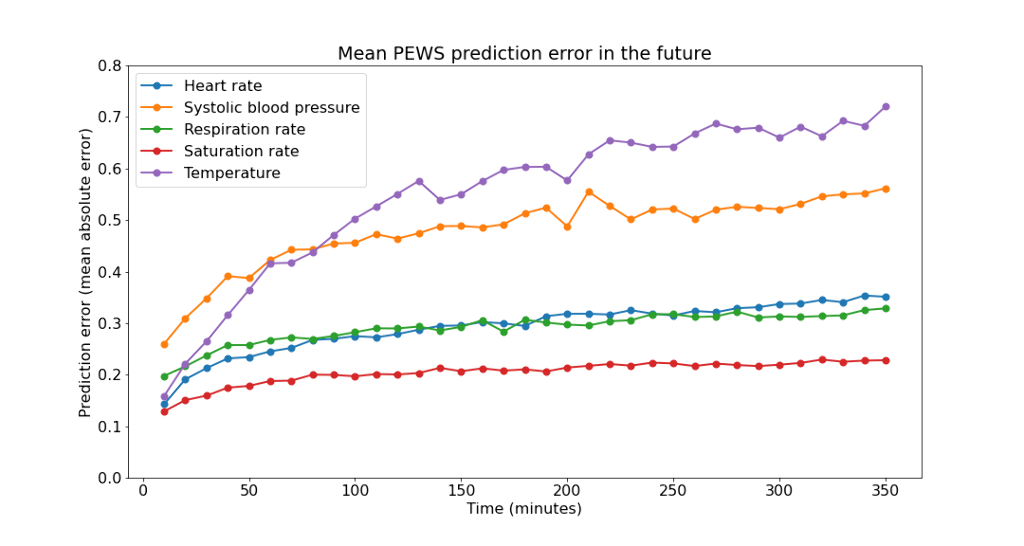
 Predictions of vital signs show reasonable errors, slightly increasing as time progresses (Figure1). The PEWS predictions are compared to the observed, calculated PEWS, showing reasonable calibration (Figure2).
Predictions of vital signs show reasonable errors, slightly increasing as time progresses (Figure1). The PEWS predictions are compared to the observed, calculated PEWS, showing reasonable calibration (Figure2).
Conclusions
Vital sign prediction at the PICU showed the first promising steps in the use of new Machine Learning strategies to optimize care.
FALL INJURIES REQUIRING PEDIATRIC INTENSIVE CARE UNIT (PICU) ADMISSIONS IN A MAJOR ACUTE HOSPITAL IN HONG KONG
Abstract
Background and Aims
Pediatric fall injuries lead to significant mortality and morbidity worldwide. This study evaluates the characteristics, treatments and outcomes of severe fall injuries that require PICU care.
Methods
A 5-year retrospective evaluation of pediatric fall injuries admitted to the PICU, Queen Elizabeth Hospital, Hong Kong between 2014 and 2018 was performed. Patient demographics, reason(s) of fall, injury severity scores (ISS), treatments, and the final disposals were collected and analyzed.
Results
68 patients (34 boys and 34 girls) were admitted to PICU due to fall injuries during the 5-year period. The median (IQR) age was 5.5 (1.5, 10.3) years old. 92.6% (63 patients) sustained unintentional fall injuries. Intentional injuries occurred in older children (aged 13.6 vs 4.9 years old, p=0.021), and resulted in more critical trauma (Injury severity score ISS 26.0 vs 17.0, p=0.013). Surgical interventions were performed in 50% of the admissions, of which 88.2% involved neurosurgical procedures. The median length of stay in PICU and hospital were 1.6 (0.9, 3.0) and 7.6 (3.8, 11.6) days respectively. Two patients did not survive to discharge. Patients with ISS >25 on admission received more surgical interventions (OR 11.2, 95%CI 2.3-54.6), blood transfusion (OR 7.1, 95%CI 2.0-24.5) and inotropic support (OR 11.4, 95%CI 1.9-66.4), and required longer hospitalization.
Conclusions
Patients with intentional falls were older in age, and sustained more severe trauma. Overall, 50% of the patients required surgical interventions, which were mostly neurosurgical procedures. More treatments and longer hospitalization were required in severe trauma with ISS >25.
CARDIAC ARREST ON PICU- THEMES, MANAGEMENT AND QUALITY OF CPR
Abstract
Background and Aims
A 6 month retrospective audit of cardiac arrests (CA) on a tertiary PICU was performed to:
Classify and review management of CA
Review whether high risk indicator criteria could have helped predict/avoid CA
Review chest compression data recorded by the defibrillators
Methods
We extracted EPR/observation data covering arrest classification, management and outcome and patient demographics. We assessed the cause of arrest for preventability. Parameters were compared to published high risk indicators. Defibrillator sensor data (compression depth and rate) was compared with RC UK guideline targets.
Results
28 CA in 20 patients over 6 months when 400 patients were admitted; incidence 5%. 50% had no high risk indicators.
Time of CA: 50% dayshift / nightshift.
Length of CA: 0.16-37 minutes
Asystole 10.7%, bradycardia 25%, PEA 50%, pulseless VT 10.7%
1 avoidable and 2 potentially avoidable CA (inotrope line disconnection, TT blockage with secretions, hypotension with sedation bolus); all survived.
Many patients not correctly admitted to monitors so physiological data inadequate.
Chest compression (CC) rate target (100-120/minute) achieved in 21.2% of compressions.
Depth CC target (infant- 4cm, child- 5cm) achieved in 9.2% of compressions.
Outcomes: ROSC achieved in 82% of CA. Of 20 patients 10 survived to hospital discharge, 5 had redirection of care, 5 did not achieve ROSC.
Conclusions
CC rate and depth needs to improve – CPR coaching, improve targeted ‘just in time’ resuscitation training for patients with high risk indicators.
Not all data streams reliably captured- patients not admitted to monitors correctly
Need for documented post ROSC care plan in medical notes.
