Welcome to the ESPNIC Xperience Programme Scheduling
The meeting will run on Central European Summer Time
PREDICTING EARLIER AND MANAGING DETERIORATION OUTSIDE THE PICU: THE CRITICAL CARE OUTREACH NURSE ROLE AND SERVICE
PEDIATRIC EARLY WARNING SCORES AND ESCALATION ALGORITHMS: DO THEY REALLY HELP?
COMPARISON OF PAEDIATRIC EARLY WARNING SCORES AND ORGAN DYSFUNCTION SCORES IN PREDICTING CRITICAL CARE ADMISSION, SEPSIS AND MORTALITY IN FEBRILE CHILDREN (FROM THE PERFORM STUDY)
Abstract
Background and Aims
Identifying life-threatening bacterial infection in febrile children presenting to the Emergency Department (ED) is challenging. Numerous different PEWS (Paediatric Early Warning Scores) are used to identify children at highest risk of deterioration, needing urgent antimicrobial treatment and resuscitation.
This study compares performance of eight PEWS and two organ dysfunction scores in predicting critical care (CC) admission, sepsis, mortality and bacterial/viral aetiology of infection, for febrile paediatric ED attendees.
Methods
In total, 2446 children were included from PERFORM, a multi-centre prospective cohort study of febrile children across Europe.
Eight PEWS (Alder Hey, Bedside, Bristol, ED-PEWS, National, Newcastle, Paediatric Observation Priority Score (POPS), Scotland) and age-adjusted quick sequential organ failure assessment (qSOFA) and Liverpool quick sequential organ failure assessment (LqSOFA) were calculated from triage observations.
Results
192 children (7.8%) were admitted to CC within 48 hours of ED presentation, 14.3% had sepsis, and 28 Day mortality was 0.3%.
Alder Hey, Bedside, Bristol, National, Newcastle, Scotland and LqSOFA demonstrate good prediction of CC admission <48 hours (AUC range 0.77-0.84) and 28-day mortality (0.76-0.89) with variable prediction of sepsis (0.69-0.80). qSOFA demonstrates poor prediction of CC admission <48 hours and sepsis (0.55-0.62) , but good prediction of 28-day mortality (0.86). ED-PEWS (0.37-0.50) and POPS (0.36-0.50) demonstrate poor prediction of these outcomes. None differentiate between bacterial/viral aetiology (0.46-0.53).
Conclusions
This study demonstrates good performance of six PEWS and LqSOFA to identify febrile children at risk of poor outcome in ED, but emphasise the need for other markers to rapidly discriminate between bacterial/viral aetiology, to improve targeted antimicrobial use.
DEVELOPING A VALIDATED FRAMEWORK FOR ASSESSING PREVENTABILITY OF PAEDIATRIC CRITICAL DETERIORATION EPISODES (CDE)
Abstract
Background and Aims
Missed or late identification of deteriorating children in hospital results in unplanned admission to critical care. Within a NIHR study to evaluate the use of SMART technology to reduce critical deterioration (DETECT study ISRCTN61279068), we developed and validated a framework for assessing preventability.
Methods
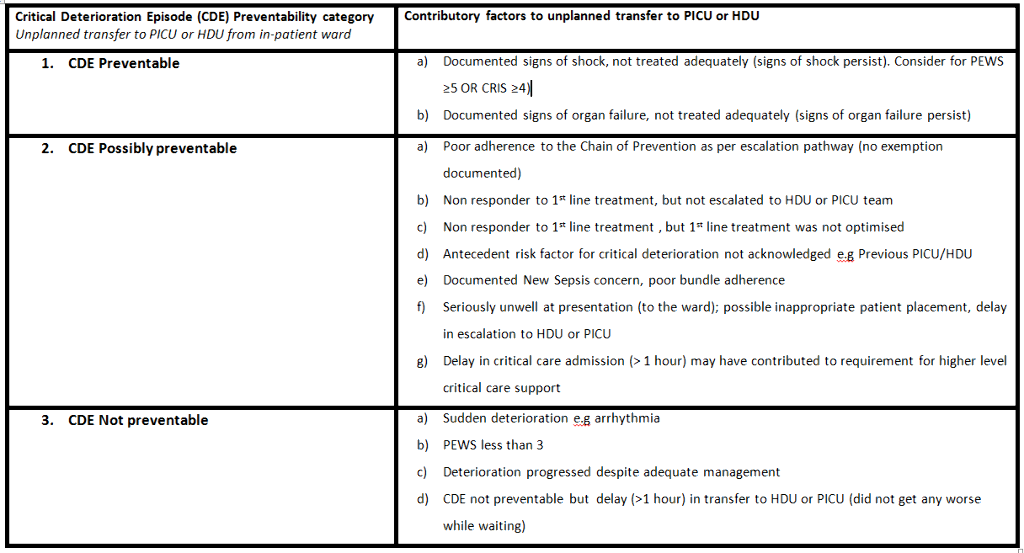
A model for assessing preventability was developed by a multi-disciplinary team incorporating patient, clinician and system factors. The framework was piloted using ten cases and the contributing factors made more explicit. The final framework was subsequently validated in a cohort of cases of unplanned admissions to PICU or HDU from in-patient wards, March to December 2018. Cases were independently reviewed by two members of a team of senior critical care nurses and a consultant. Vital signs, drug charts, nursing and medical documentation were reviewed. The contributing factors of the CDE were identified, and an overall preventability categorisation applied. Disagreements were resolved by a third independent reviewer. A minimum of two in agreement was required.
Results
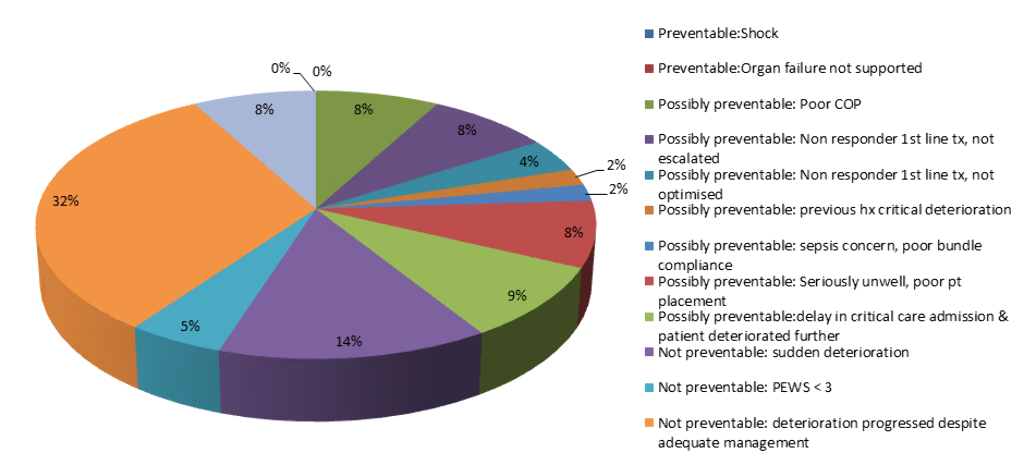
253 cases were reviewed. Inter-rater reliability was 85% agreement of preventability categorisation by two reviewers, rising to 97% with a 3rd review of 37 cases. 58% (n=147) of CDE were not preventable, 41% (n=104) potentially preventable and 1% were preventable (n=2). Factors contributing to the unplanned transfer to critical care were collated.
Conclusions
A structured framework for reviewing preventability of in-hospital deterioration had strong inter-rater reliability. Collating the contributing factors provided shared learning about the patient, clinician and system factors that could be used to mitigate future risk in managing in-patient deterioration.
USING QUALITY IMPROVEMENT (QI) METHODOLOGY TO CREATE A UNIT-BASED APPROACH TO DECREASING RATE OF UNPLANNED EXTUBATIONS IN PAEDIATRIC INTENSIVE CARE
Abstract
Background and Aims
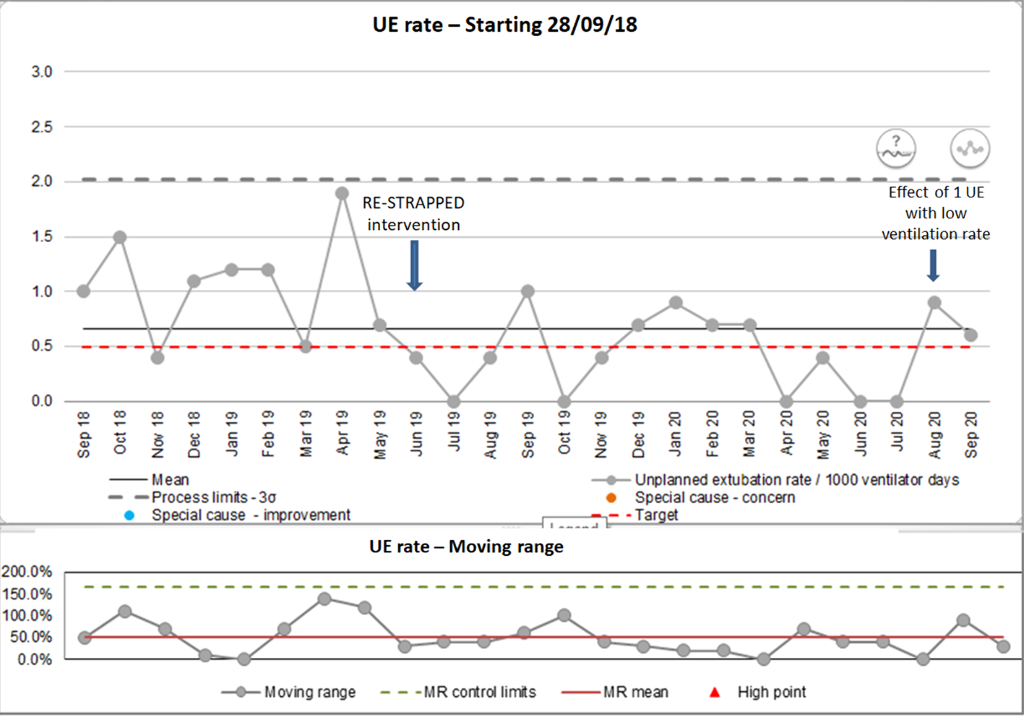
Unplanned extubation (UE) in the paediatric intensive care unit (PICU) is a well-recognised complication of invasive mechanical ventilation. Its consequences can be severe including airway trauma and death. A PICU’s UE rate is used as an indicator of unit safety. All UK PICUs report their UE rates per 1000 ventilator days (UE/1000Vd) with a target set at <1.0UE/1000Vd. To help achieve this target we used a QI approach. We created a UE bundle to investigate the problem, deliver education, change culture, monitor performance and improve our patient care.
Methods
We created a UE bundle with a multi-faceted approach. Core components focussed on:
• Guideline development
--RE-STRAPPED approach (acronym), care for endotracheal tubes (ETTs) and alternative methods for securing them
• Education
-- Nursing/medical staff education, targeted posters and compulsory competency based training on securing an ETT
• Cultural change
--Empowering nurses – re-securing now primarily a nursing role and zero tolerance approach to unsecure ETTs
-- RE-STRAPPED champions available on every shift
• Performance monitoring
-- New tools to document securing of ETT and Datix collection tool to monitor events
-- Performance reviewed at monthly governance meetings with action points
Results
We demonstrated a mean reduction of UEs from 0.99UE/1000Vd [+/- 0.25] in the 10 months prior to our intervention to 0.45 UE/1000Vd [+/- 0.14] in the 15 months post intervention (t-test calculation, assuming equal distribution, p=0.005).
UE statistical process control chart:
Conclusions
Through continuous quality improvement and an education program we were able to implement a statistically significant change in rates of UE.
AN INTERVENTION TO IMPROVE PATIENT SAFETY AWARENESS IN A PEDIATRIC INTENSIVE CARE UNIT OF A TERTIARY UNIVERSITY HOSPITAL IN MADRID, SPAIN
Abstract
Background and Aims
Patient safety is one of the six dimensions of healthcare quality. Is a growing challenge and has become a priority. National organizations promote policies and programs to enhance patient safety culture. Reporting systems are recommended to identify, analyze and mitigate hazards.
Clinical practice is a combination of processes, technologies and human interactions that leads to a risk for adverse events.
We aim to assess the impact of an intervention to promote safety culture and improve incident reporting.
Methods
During July and September 2020, safety medical team recorded incidents in ward rounds. Compared with those reported by institutional electronic notification system for safety related events (SINOIRES®), the rate of notification was significantly lower (8 notifications vs 23 incidents discussed).
An intervention was developed to motivate patient safety awareness. A new section was included in ward rounds. Voluntary notification was encouraged.
Notifications and interventions after 2 months (November-December 2020) are described.
Results
61 adverse effects have been notified by SINOIRES® and 73 discussed during wards.
Notifications are classified in: communication, prescription or administration errors, nosocomial infections, delirium, accidental extubation, loss of devices, equipment related adverse effects and others. The majority were equipment related (29.5%) followed by communication (22.95%) and prescription errors (18%). 19 interventions have been initiated. Events and its interventions have been reported weekly to the unit.
Conclusions
This intervention has made the team more aware of patient safety in daily practice by making risks more visible. Has allowed us to minimize adverse events frequency and reduce patient harm. Long term follow up is required.
MACHINE LEARNING ON PAEDIATRIC INTENSIVE CARE DATASETS TO IMPROVE MORTALITY PREDICTION MODELS
Abstract
Background and Aims
Paediatric intensive care unit (PICU) mortality prediction models, such as the Paediatric Index of Mortality (PIM) are historically based on manual data entry and retrieval. Presently, Electronic Medical Record (EMR) systems contain more detailed and/or more frequently measured data. The aim of this study was to assess whether machine learning (ML) on PICU datasets extracted from the EMR outperform existing mortality prediction models.
Methods
Data from patients admitted to the PICU of the University Medical Center Utrecht, The Netherlands, between 2009 and 2018 were collected. Variables from existing prediction models (PIM2, PIM3, Paediatric Risk of Mortality (PRISM) III) were extracted from the local Dutch PICU quality registry (PICE), whereas vital signs and laboratory values were extracted from a local PICU research data warehouse. Logistic regression, support vector machines and random forest were fitted on the dataset using hold-out validation. Variables were selected both manually as via algorithms. All existing and ML models were evaluated by comparing their areas under the receiver operating characteristics (AUROCs).
Results
PIM3 was the best performing existing mortality score with an AUROC of 88% [95%CI 81%-90%]. The AUROC’s of the different tested ML methods, pre-processing, and hyperparameter combinations fluctuated heavily (30%-90%). Logistic regression had superior performance with an AUROC 93.1% [95%CI 91%-95%] fitted on the PICE dataset in combination with laboratory values.
Conclusions
Interpretable ML models can improve existing prediction models on PICU mortality, with the addition of EMR data. Further improvement of the models with real time predictions could improve clinical application.
