
Luregn J. Schlapbach (Switzerland)
Author Of 9 Presentations
PROGRESSION OF ACUTE KIDNEY INJURY IN CRITICALLY ILL CHILDREN
Abstract
Background and Aims
Acute kidney injury (AKI) is common in critically ill children. We sought to describe the prevalence and progression of AKI in critically ill children.
Methods
This was a retrospective observational study conducted in a multi-disciplinary Paediatric Intensive Care Unit (PICU) from January 2015 to December 2018. All children from birth to ≤16 years old who were admitted to the PICU were included. We used the Kidney Disease: Improving Global Outcomes (KDIGO) criteria as AKI reference standard. The progression of patients with AKI were followed through the first 7 days of PICU admission. Patients were defined as Early AKI if AKI was present within 48 hours of admission. Recovery from AKI was defined as not fulfilling KDIGO criteria from 48 hours until seven days of admission while partially recovered from AKI were defined as a reduction from a higher stage to lower stage of AKI in the same period.
Results
The prevalence of AKI in our cohort (n=7505) was 9.2%. There were 554 (7.4%) children who had Early AKI. Recovery from Early AKI was seen in 70.4% of these children while 1.4% had partial recovery (Figure 1). Worsening of stage of AKI was observed in 6.5% (n=36) of these children. Out of these children who progressed to a worse stage, 36% (n=13) died.

Conclusions
Nearly one in ten children admitted to our PICU had AKI as defined by KDIGO. AKI persisted beyond seven days in one third of these children. Further studies are needed to follow-up patients with persistent AKI at hospital discharge.
CHAIRPERSON INTRODUCTION
CHAIRPERSON INTRODUCTION
TOWARDS A EUROPEAN NICU AND PICU DATA SHARING FRAMEWORK: AN ESPNIC INITIATIVE
Abstract
Background and Aims
A framework to safely share clinical data from European Pediatric and Neonatal Intensive Care Units (PICU, NICU) will enhance research, improve clinical benchmarking and promote quality improvement projects among participating centres. When applying advanced data science methods such as machine learning to heterogenous patient data, substantial amounts of patient data from different centres may be needed to produce and validate reliable models.
The aim of this research is to summarize conditions and requirements which such a framework must meet in order to take the first steps towards a European NICU and PICU clinical data framework.
Methods
A survey was conducted among the members of the ESPNIC Data Science Working Group to investigate the use of electronic medical records (EMR) among European NICU’s and PICU’s and to identify European experts in NICU and PICU data registries and data science. During three meetings, these experts defined a list of topics regarding the framework conditions and requirements.
Results
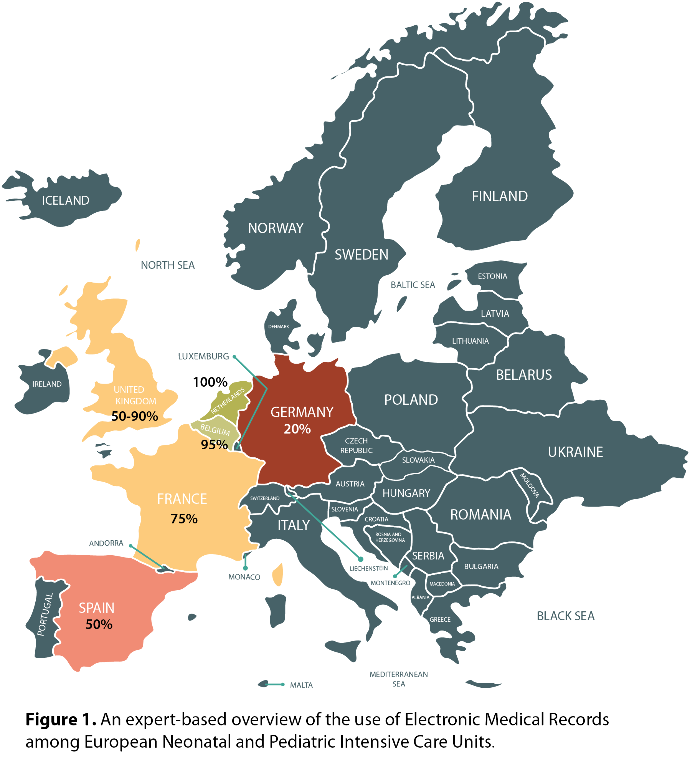
The use of EMR ranged from approximately 20% in Germany to 100% in The Netherlands (Figure 1). Fourteen European experts in data registries and data science were identified. They reached consensus on the requirements for a European NICU and PICU data framework, which included data availability, data standardization, legislation and privacy, funding and framework architecture.
Conclusions
Several requirements for a European NICU and PICU clinical data sharing framework were identified, including data availability. The variable use of EMR among European centres may detain development of such a framework.
EDUCATIONAL OUTCOMES AT SCHOOL AGE IN CHILDHOOD SURVIVORS OF CRITICAL ILLNESS
Abstract
Background and Aims
Approximately 2 out of 1000 children require critical care support, but little is known about the impact of critical illness into school performance. While major post-intensive care sequelae affect up to one in three adult survivors of critical illness, similar data for critically ill children are lacking.
We aimed to determine primary school educational outcomes in children who required admission to PICU during childhood.
Methods
Multicentre population-based linkage study. Children <5 years old admitted to PICU in Queensland, Australia, between 1997 and 2016 were eligible if they had survived until the age of NAPLAN testing. Using the National Assessment Program – Literacy and Numeracy (NAPLAN) database, the primary outcome was defined as educational achievement below the National Minimum Standard (NMS) in year 3 of primary school.
Results
Primary school data were available for 5,017 PICU survivors (median age 8.0 months at first PICU admission). PICU survivors scored significantly lower than controls across each domain (p<0.001). 14.03% of PICU survivors did not meet the NMS, compared to 8.96% of matched controls (p<0.001). In multivariate analyses, socioeconomic status (OR 2.14; 95%-CI 1.67-2.74), logit of Pediatric Index of Mortality-2 score (1.11; 1.03-1.19), and presence of a syndrome (11.58; 8.87-15.11) were some of the key predictors of not meeting the NMS.
Conclusions
In this study of childhood PICU survivors, 14.03% did not meet national minimum standards in the standardized primary school assessment. Socioeconomic status, underlying diseases, and severity on presentation allow risk-stratification to identify children most likely to benefit from individual follow-up and support.
WE REALLY NEED A NEW PAEDIATRIC SEPSIS DEFINITION
CHAIRPERSON INTRODUCTION
HYDROCORTISON, VITAMINS & CO - JUST ANOTHER MAGIC BULLET MISSING THE TARGET?
Presenter of 7 Presentations
HYDROCORTISON, VITAMINS & CO - JUST ANOTHER MAGIC BULLET MISSING THE TARGET?
CHAIRPERSON INTRODUCTION
CHAIRPERSON INTRODUCTION
EDUCATIONAL OUTCOMES AT SCHOOL AGE IN CHILDHOOD SURVIVORS OF CRITICAL ILLNESS
Abstract
Background and Aims
Approximately 2 out of 1000 children require critical care support, but little is known about the impact of critical illness into school performance. While major post-intensive care sequelae affect up to one in three adult survivors of critical illness, similar data for critically ill children are lacking.
We aimed to determine primary school educational outcomes in children who required admission to PICU during childhood.
Methods
Multicentre population-based linkage study. Children <5 years old admitted to PICU in Queensland, Australia, between 1997 and 2016 were eligible if they had survived until the age of NAPLAN testing. Using the National Assessment Program – Literacy and Numeracy (NAPLAN) database, the primary outcome was defined as educational achievement below the National Minimum Standard (NMS) in year 3 of primary school.
Results
Primary school data were available for 5,017 PICU survivors (median age 8.0 months at first PICU admission). PICU survivors scored significantly lower than controls across each domain (p<0.001). 14.03% of PICU survivors did not meet the NMS, compared to 8.96% of matched controls (p<0.001). In multivariate analyses, socioeconomic status (OR 2.14; 95%-CI 1.67-2.74), logit of Pediatric Index of Mortality-2 score (1.11; 1.03-1.19), and presence of a syndrome (11.58; 8.87-15.11) were some of the key predictors of not meeting the NMS.
Conclusions
In this study of childhood PICU survivors, 14.03% did not meet national minimum standards in the standardized primary school assessment. Socioeconomic status, underlying diseases, and severity on presentation allow risk-stratification to identify children most likely to benefit from individual follow-up and support.
