Welcome to the ESOC 2021 Virtual Conference Calendar
The Conference will officially run on Central European Summer Time (GMT/UTC+2). To convert the conference time to your local time - Click Here
The viewing of sessions cannot be accessed from this conference calendar.
All sessions are accessible via the Main Lobby on the Virtual Platform.
 ESOC TV
ESOC TV  On Demand Session (watch anytime)
On Demand Session (watch anytime)  Pre-recorded Session with Live Q&A
Pre-recorded Session with Live Q&A
 Session with Voting
Session with Voting  Live Session
Live Session
Introduction by the Convenors
MULTIPARAMETRIC MODEL FOR PREDICTION OF ACTIVE MALIGNANCY IN STROKE PATIENTS
Abstract
Background And Aims
To detect occult malignancy which determines early treatment decisions, patient outcome and guidance of secondary prevention as a stroke etiology, we aimed to develop a multiparametric predictive model of malignancy-related stroke based on associated biomarkers.
Methods
Single-center cross-sectional study including consecutive first-ever ischemic stroke patients treated between July 2017 and November 2018. After identification of patients with a diagnosis of active malignancy before index-stroke (known malignancy) and 1-year thereafter (occult malignancy), Lasso analysis of logistic regression and cross-validation by bootstrapping were used to determine discrimination and calibration of prespecified clinical variables and biomarkers for active malignancy.
Results
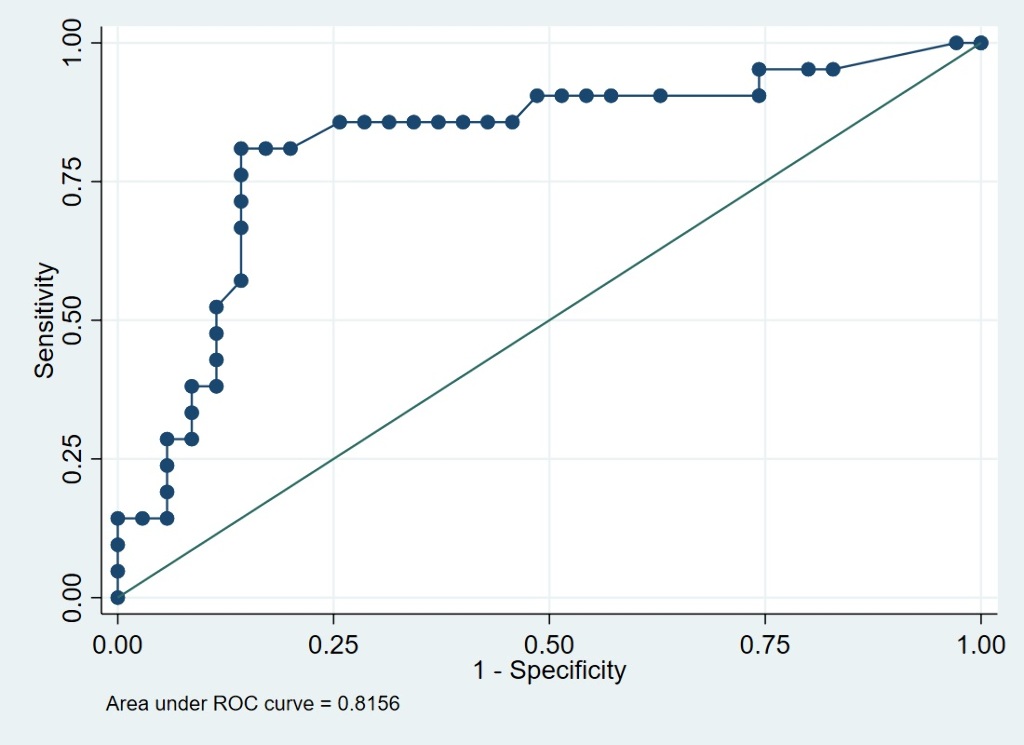
Among 1001 patients with first ischemic stroke, 61 patients (6.09%) had an active malignancy. Out of those, 39 patients (64%) had a known malignancy and 22 patients (36%) had an occult malignancy. The final risk algorithm for active malignancy included multi-territorial infarcts (aOR 2.4, 95% CI 1.3- 4.6, P=0.006), anemia (aOR 4.2, 95% CI 1.6 – 11, P=0.003), elevated D-dimer levels (aOR 3.1, 95% CI 1.1 – 9.0, P=0.034) and male sex (aOR 1.9, 95% CI 1.0 – 3.4, P=0.042). The area under the Receiver Operating Characteristic curve of the selected multiparametric model was 0.8156 (Figure 1).
Conclusions
The combination of malignancy-related stroke biomarkers increases the prediction of underlying malignancy in stroke patients and may improve the detection of occult malignancy at the index-hospitalisation. Prospective studies for validation of a predictive score and identification of other malignancy-related biomarkers in stroke-patients are needed.
THE GRAZ AF RISK SCORE: A BIOMARKER-BASED APPROACH TO PREDICT ATRIAL FIBRILLATION AFTER CRYPTOGENIC STROKE
Abstract
Background And Aims
Atrial fibrillation (AF) often remains undiagnosed in cryptogenic stroke (CS), mostly because of limited availability of cardiac long-term rhythm monitoring. There is an unmet need for a pre-selection of CS patients benefiting from such work-up. We therefore developed a clinical risk score to predict AF after CS and evaluated its performance over one year of follow-up (FU).
Methods
Our proposed risk score ranges from 0 to 16 points and comprises variables known to be associated with occult AF in CS patients including age, NT-proBNP, electro- and echocardiographic features (supraventricular premature beats, atrial runs, atrial enlargement, left ventricular ejection fraction) and brain imaging markers (multi-territory/prior cortical infarction). We prospectively followed all CS patients admitted to the Stroke Unit of the University Clinic of Neurology in Graz from March 2018 to August 2019 for AF detection over one year after discharge.
Results
During FU, we diagnosed 24 (16%) out of 150 CS patients with AF (detected via ECG-controls, n=18; loop recorder-monitoring, n=6). Our predefined AF risk score (cutoff ≥4 points; highest Youden’s Index) had a sensitivity of 92% and a specificity of 68% for one-year prediction of AF. Notably, only two CS patients with <4 score points were diagnosed with AF later on (negative predictive value: 98%).
Conclusions
We here present a clinical AF risk score for one-year prediction of AF in CS with high sensitivity, reasonable specificity, and excellent negative predictive value. Generalizability of our score needs to be tested in external cohorts with continuous cardiac rhythm monitoring.
Trial Registration Number
not applicable
MIND THE HEART: ECG-GATED CARDIAC COMPUTED TOMOGRAPHY IN ACUTE ISCHAEMIC STROKE
Abstract
Background And Aims
CT of the heart and aortic arch performed in the acute phase of ischaemic stroke is a promising diagnostic tool for detection of cardio-aortic sources of embolism.
Methods
We performed a single-center, prospective cohort study in consecutive adult patients with acute ischaemic stroke. Patients underwent prospective sequential electrocardiography-gated cardiac CT-angiography, immediately after CT-angiography of the aortic arch, cervical and intracranial arteries. Patients also underwent routine stroke work-up, including transthoracic echocardiography (TTE). Primary endpoint was the proportion of patients with a predefined high-risk cardio-aortic source of embolism on CT versus TTE in patients undergoing both investigations. Based on an expected 5% additional yield of CT and assuming 75% of included patients would undergo both CT and TTE, a sample size of 450 patients was required.
Results
452 patients (59.2% male, median age 72) were included and underwent cardio-aortic CT. Of these, 349 (77.2%) also underwent TTE. In these 349 patients, the diagnostic yield for high-risk cardio-aortic sources of embolism was 11.7% for CT compared to 4.8% for TTE (McNemar mid-p <0.001). Cardiac thrombus was the most frequent CT finding (40 patients [8.8%], table 1). Among 97 patients (21.5%) with an embolic stroke of undetermined source based on routine stroke work up, seven (7.2%) had a high-risk source of embolism on cardio-aortic CT.
Conclusions
Cardio-aortic CT acquired in the acute phase of ischaemic stroke has a higher diagnostic yield for high-risk cardio-aortic sources of embolism than TTE and will thus reduce the proportion of patients with cryptogenic stroke.
Trial Registration Number
NA
“RED CARDIAC VERSUS WHITE ATHEROSCLEROTIC THROMBOEMBOLI IN ACUTE ISCHEMIC STROKE”: CHALLENGING THE CONCEPT VIA A LARGE-SCALE, DETAILED MULTI-PARAMETRIC HISTOLOGICAL ANALYSIS
Abstract
Background And Aims
Stroke thromboemboli are often described as white (platelet-rich) or red (red blood cell (RBC)-rich) when having an atherosclerotic or cardiac origin respectively. Secondary stroke prevention is mainly based on antiplatelet therapy for atherosclerotic etiologies and anticoagulation for cardioembolic etiologies. Yet, up to 25% of patients still experience a recurrent stroke. Better understanding of thromboembolus composition can improve our understanding of underlying pathophysiologies and potentially improve prevention strategies. The aim was to perform a large-sample multi-parameter quantitative histological analysis to investigate differences in thromboembolus composition of different etiologies.
Methods
Thromboemboli (n=501) were collected from thrombectomy-treated ischemic stroke patients at Groeninge Hospital (Kortrijk, Belgium) and CHU Lille (Lille, France). Stroke etiology was categorized according to the TOAST classification. Histological analysis was performed for the amount RBCs, platelets, fibrin, von Willebrand factor (VWF), leukocytes, citrullinated histone H3 (H3Cit) and extracellular (ex)DNA.
Results
Compared to large-artery atherosclerotic (LAA) thromboemboli (Fig.1), cardioembolic (CE) thromboemboli contained significantly less RBCs and significantly more platelets, fibrin, leukocytes and exDNA. VWF and H3Cit content were similar in CE/LAA thromboemboli. Cryptogenic thromboemboli contained relatively low amounts of RBCs and high amounts of platelets (Fig.1), similar to CE thromboemboli. Notwithstanding these population differences, a typical CE or LAA thromboembolus cannot be defined given the heterogeneity in RBC/platelets.
Conclusions
In contrast to current concepts of ‘white’ atherosclerotic and ‘red’ cardiac thrombi, CE thromboemboli are more platelet-rich compared to RBC-rich LAA thromboemboli, with a heterogenous RBC/platelet thrombus profile. Such data could hint at combining antiplatelet with anticoagulation therapy in stroke prevention, as shown in the COMPASS-trial.
Trial Registration Number
Not applicable
THROMBI WITH LOW PERCENTAGE OF CD4 MAY INDICATE ATRIAL FIBRILLATION AS THE SOURCE OF THE STROKE
Abstract
Group Name
ITACAT study group
Background And Aims
We performed a histological and immune analysis of the clot in acute stroke patients to determine predictors of atrial fibrillation (AF).
Methods
We conducted a prospective observational study of consecutive patients with acute stroke who underwent thrombectomy that obtained extracted thrombus (ITACAT study). Several staining were performed to evaluate red blood cells/fibrin (hematoxylin/eosin), platelets (CD61) and leucocytes (CD4, CD8 and CD20). All patients received CT angio to detect extra/intracranial vascular stenosis and 30-day cardiac monitoring to diagnose AF. Thrombi were classified in stroke due to AF (T-AF), due to symptomatic atherosclerosis (T-AT) and without any cause (T-CRYP). We excluded strokes due to double cause or incomplete workup.
Results
Of the 215 patients: 69 were T-AT, 101 were T-AF and 45 were T-CRYP. There was no difference in percentage of hypertension, diabetics and hypercholesterolemia. Percentage of AF detection was: 3% (2/65) in T-AT, 100% (101/101) in T-AF and 40% (18/45) in T-CRYP. T-AF patients were older: T-AF 79 years (70-84) Vs. T-AT 68 years (60-76) Vs. T-CRYP 70 years (53-78) (p=0.001). T-AT group had a greater percentage of CD4: T-AT 6.76% (4-13) Vs. T-AF (3.67% (2-7) Vs.T-CRYP 4.14% (2-13) (p=0.033) and a fewer percentage of CD61: T-AT 51.33% (33-69) Vs.AF 70.62% (51-83) Vs. CRYP 69.54% (61-87) (p=0.007). The age (OR 1.47 (1.10-2) (p=0.011) and the percentage of CD4 (OR 0.83 (0.69-0.98) (p=0.034) were independently associated with AF detection. Final analysis (n=400 cases) will be ended in September 2021.
Conclusions
Patients with AF detection in work up had lower percentage of CD4 in extracted thrombi.
Trial Registration Number
Not applicable
CIRCADIAN RHYTHM OF ISCHEMIC CORE PROGRESSION IN HUMAN STROKE
Abstract
Background And Aims
Experimental stroke studies suggest an influence of the time of day of stroke onset on infarct progression (Esposito et al. Nature 2020). Whether this holds true after human stroke is unknown, but would have implications for the design of randomized controlled trials, especially those on neuroprotection.
Methods
We pooled data from 583 patients with anterior large-vessel occlusion stroke from three prospectively recruited cohorts. Ischemic core and penumbra volumes were determined with CT perfusion using automated thresholds. Core growth was calculated as the ratio of core volume and onset-to-imaging time. To determine circadian rhythmicity, we applied multivariable linear and sinusoidal regression analysis adjusting for age, onset-to-imaging time, collateral score, and center.
Results
Patients with symptom onset at night showed larger ischemic core volumes upon admission compared to patients with onset during the day (median, 40.2 ml vs. 33.8 ml), also in adjusted analyses (p=0.008). Sinusoidal analysis indicated a peak of core volumes with onset at 11pm. Core growth was faster at night compared to day onset (adjusted p=0.01), especially for shorter onset-to-imaging times. In contrast, penumbra volumes did not change across the 24-h cycle.
Conclusions
These results suggest that human infarct progression varies across the 24-h cycle with potential implications for the design and interpretation of neuroprotection trials.
Trial Registration Number
Not applicable
PREDICTORS AND CLINICAL IMPACT OF INFARCT PROGRESSION RATE IN THE ESCAPE-NA1 TRIAL
Abstract
Group Name
on behalf of the ESCAPE-NA1 investigators
Background And Aims
Determining infarct progression rate in acute ischemic stroke (AIS) is important for patient triage, treatment decision-making and outcome prognostication. We estimated infarct progression rate in AIS patients with large vessel occlusion (LVO) and determined its predictors and impact on clinical outcome.
Methods
AIS patients with time from last-known-well-to-randomization<6h and near-complete reperfusion following EVT (eTICI 2c/3) were included in this study. Infarct growth rate (mL/h) was estimated by dividing 24h infarct volume (measured on NCCT or DWI-MRI) by time from last-known-well-to-reperfusion. Multivariable linear regression was used to assess the association of patient baseline variables with log-transformed infarct progression rate. The association of infarct progression rate and good outcome (mRS 0-2 at 90d) was determined using multivariable logistic regression.
Results
Four-hundred-two patients were included in the study. Median infarct progression rate was 4.73 mL/h (IQR:1.24-14.85). Collateral status (β:-0.83[95%CI:-1.22;-0.44]), Alberta Stroke Program Early CT-Score (ASPECTS,β:-0.35[95%CI:-0.47;-0.24]) and National Institutes of Health Stroke Scale (NIHSS,β:0.07[95%CI:0.04;0.10]) were associated with log-transformed infarct progression rate. Patients’ clinical and imaging baseline variables explained 20% of the variance in infarct progression rate. Infarct progression rate was significantly associated with good outcome (aOR per 1mL/h increase: 0.96[95%CI:0.95;0.98], see figure).
Conclusions
In this sample of early time window LVO-patients who underwent successful recanalization, infarct progression rate was inversely correlated with good clinical outcome. While a significant association between ASPECTS, collateral status and NIHSS and infarct progression rate was observed, these baseline imaging and clinical characteristics explained only a small proportion of the inter-individual variance, suggesting the need for more research on measurable factors affecting infarct growth.
Trial Registration Number
NCT02930018
DIFFERENCES IN INFLAMMATORY PROFILES BETWEEN YOUNG AND OLDER PATIENTS WITH STEMI OR ACUTE ISCHEMIC STROKE
Abstract
Background And Aims
Aging is associated with a chronic low-grade inflammatory state. This condition may affect the acute inflammatory response involved in ST-elevation myocardial infarction (STEMI) or acute ischemic stroke (AIS). We sought to compare the profile of a set of circulating inflammatory markers between young and older patients admitted for AIS or STEMI.
Methods
HIBISCUS-STROKE and HIBISCUS-STEMI cohorts included AIS patients treated with mechanical thrombectomy and STEMI patients treated with primary percutaneous coronary intervention, respectively. Age cut-off was 65 years. In both cohorts, C-reactive protein (CRP), interleukin (IL)-6, IL-8, IL-10, monocyte chemoattractant protein-1 (MCP-1), soluble tumor necrosis factor receptor I (sTNF-RI), soluble form suppression of tumorigenicity 2 (sST2) and vascular cellular adhesion molecule-1 (VCAM-1) were measured on serum collected at 5 time-points using ELISA. A multiple logistic regression model was performed to detect an association between area under the curve (AUC) of circulating inflammatory markers within the first 48 hours and older age.
Results
A total of 164 AIS and 260 STEMI patients were included. Of them, there were 105 (64%) and 76 (30%) older AIS and STEMI patients, respectively. Following multivariate analysis, a high AUC of IL-6 and sTNF-RI, a low lymphocyte count and a high neutrophil lymphocyte ratio (NLR) at 24 hours were associated with older age in AIS and STEMI patients.
Conclusions
Older patients had higher IL-6 and sTFN-RI levels within the first 48 hours associated with a low lymphocyte count and a high NLR at 24 hours in both cohorts.

