Welcome to the ATTD 2022 Interactive Program
The conference will officially run on Central European Summer Time (UTC+2) - Barcelona Time
To convert the conference times to your local time Click Here
DIABETES NOVEL SUBGROUP ASSESSMENT (DIANA)- ADVANCED MACHINE LEARNING-BASED TOOL TO CLASSIFY INDIVIDUALS WITH NEWLY DETECTED TYPE 2 DIABETES INTO SPECIFIC SUBGROUPS AND ASSESS DRUG RESPONSE
Abstract
Background and Aims
Machine learning (ML) has been applied to many aspects of medical health. In this study, we aimed to develop a tool to classify individuals with newly detected type 2 diabetes(T2D) into specific subgroups recently identified in Indians.
Methods
The DIAbetes Novel subgroup Assessment (DIANA) tool has been developed in R-Shiny. The tool has been trained and tested using unsupervised ML model (K-means clustering with k value of 4 using k-means function(max iteration=10 000) in R V.3.6.0 in a dataset of 19,084 individuals with T2D (aged 10–97 years) with diabetes duration of <5 years at the time of first clinic visit. Age at onset of diabetes, BMI, waist circumference, Hba1c, serum triglycerides, serum high-density lipoprotein cholesterol, fasting and stimulated C-peptide were used in this ML approach. Distinctly labelled clusters were trained using supervised ML algorithms for prediction.
Results
Four novel subgroup clusters of T2D were identified using the tool: Severe Insulin Deficient Diabetes (SIDD), Insulin Resistant Obese Diabetes (IROD), Combined Insulin Resistant and Deficient Diabetes (CIRDD) and Mild Age-Related Diabetes (MARD). There was high concordance between the un-supervised and supervised ML approaches(Cohen’s Kappa Statistic, 0.99) with 99% of prediction accuracy(83% accuracy if C-Peptide was not included in the model).
Conclusions
Identification of phenotypic subgroups of T2D using the DIANA tool, developed based on real world clinical data, could help clinicians understand aetiology of T2D and with the help of additional individualised prediction models, decide upon the most effective forms of therapy for the patient, an important first step towards precision/ personalised diabetes care.
PREDICTING HYPOGLYCEMIA AND IDENTIFYING RISK FACTORS DURING AND FOLLOWING PHYSICAL ACTIVITY IN TYPE 1 DIABETES USING EXPLAINABLE MODELS
Abstract
Background and Aims
Glucose during physical activity (PA) is highly variable among people with T1D oftentimes leading to increased hypoglycemia risk. We used explainable mixed-effects models to (1) learn key factors associated with short- and long-term PA-related hypoglycemia and (2) predict hypoglycemia in the 24-hours after start of exercise.
Methods
We leveraged the free-living Tidepool Big Data Donation Dataset (Tidepool, Palo Alto, CA, USA) comprised of time-matched continuous glucose measurement, insulin, and PA data from 50 people with T1D (6,448 PA sessions; training: 5,457 and validation: 991). We fitted mixed-effects logistic regression (MELR) and random forest (MERF) models to predict the probability of hypoglycemia during and up to 24 hours following PA. We assessed model accuracy using area-under-the-curve (AUC).
Results
There was no significant difference in accuracy between MELR and MERF. AUCs on the validation dataset were AUCMIXED=0.83, and AUCFIXED=0.65. Both models showed overall hypoglycemia risk peaking one hour and 5-10 hours after PA. Key risk factors significantly associated with hypoglycemia included glucose and insulin-on-board at start of PA, low blood glucose index 24-hours before PA, and exercise duration and intensity. Time effects differed between strength and other types of PA.
Conclusions
Results from this study can be used for decision support and insulin delivery scheduling in automated delivery systems to mitigate PA-related hypoglycemia. Significance of random effects indicates that personalization and modeling the correlation between the hours after the same PA session to capture probability of repeat hypoglycemia may help improve accuracy of hypoglycemia prediction following PA.
MEAL DETECTION AND SIZE ESTIMATION USING MACHINE LEARNING: TOWARDS FULLY AUTOMATED INSULIN DELIVERY SYSTEMS
Abstract
Background and Aims
We present a multioutput fully connected neural network model that detects meals and estimates carbohydrate content using continuous glucose monitoring (CGM) and insulin data in type 1 diabetes (T1D) both in-silico and on a real-world dataset.
Methods
The algorithm detects meals less than 60 minutes after intake. Input features were derived from 2-hour history of CGM, insulin-on-board 60 minutes prior to prediction time, and time of day. We used the UVA-Padova and the Oregon Health and Science University (OHSU) simulators for algorithm development. We simulated 100+99 virtual subjects during 14 days under real-world meal scenarios. Glucose control was simulated using the OHSU’s model predictive control (MPC) automated insulin delivery system. Dataset split was 60:40 for algorithm development and validation, respectively. The Tidepool Big Data Donation dataset (150 closed-loop users) was used for validation on real-world meal data.
Results
In-silico results showed the algorithm detected 94.70% of higher-carbohydrate meals (72.33±30.10 g, tdetection=22.9 min) with 0.11 false-positives/day (FPD) and 65.44% of lower-carbohydrate meals (46.54±26.96 g, tdetection=27.5 min) with 0.26 FPD. On the Tidepool dataset, the algorithm detected 82.48% meal candidates with 0.78 FPD. When used in a fully automated closed-loop in-silico trial, automated meal detection improved time-in-target-range (70-180 mg/dL) from 71% (no dosing for meals) to 77% (automated meal detection), < 2% time in hypoglycemia.

Conclusions
An accurate meal detection and meal size estimation algorithm can facilitate fully automated insulin delivery and improve time in range maintaining percent time in hypoglycemia < 2% on average in T1D.
REMOTE PATIENT MONITORING IN YOUTH WITH TYPE 1 DIABETES (T1D) PREDICTED TO EXPERIENCE A RISE IN A1C%: COMPARISON TO A CLINIC-DERIVED, PROPENSITY SCORE-MATCHED CONTROLS
Abstract
Background and Aims
To determine if 1) remote patient monitoring (RPM) can improve glycemic control among youth with T1D who are predicted to experience a rise in A1c% using logistic regression and 2) propensity-score (PS) matching (PSM) RPM youth to non-RPM youth can control for confounding bias.
Methods
We collected data from 2-18-year-olds attending a tertiary care network of diabetes clinics in the Midwestern USA from 11/2018-9/2021. Eligible youth had baseline A1c% ≥7.2, predicted 90-day rise in A1c% ≥0.3 via advanced machine learning, and follow-up A1c% measured 70-180 days after baseline. Criteria used to calculate PS included sex, ethnicity, race, insurance, technologies, age, T1D duration, baseline A1c%, and predicted 90-day A1c% change. We compared each RPM-youth with three matched, non-RPM youth identified using a PS within ±0.05.
Results
We matched 201 non-RPM youth to 67 RPM youth. The final cohort was 60% female, 4% Hispanic, 76% White, 54% private insurance, 37% on CGM and insulin pump, median age 13.4 years (IQR=10.3,16.0), T1D duration 44.6 months (17.6,84.7), baseline A1c% 7.9 (7.5,8.8), and predicted 90-day A1c% change 0.39 (0.33,0.48). After PSM, we found no significant differences for RPM and non-RPM youth (p’s=0.10-0.99), suggesting this method may be appropriate for creating a balanced clinic-derived control sample. However, 64% of RPM youth experienced no rise in A1c ≥0.3% compared to 53% of non-RPM youth (p=0.10).
Conclusions
Youth receiving RPM may experience improved glycemic control relative to a clinic-derived control sample based on PSM, but these results require verification in a large multisite traditionally controlled study.
REAL LIFE ESTIMATION OF POSTPRANDIAL GASTRIC RETENTION, GLUCOSE ABSORPTION AND INSULIN SENSITIVITY IN TYPE 1 DIABETES USING MINIMALLY INVASIVE TECHNOLOGIES AND COMPUTATIONAL MODELING
Abstract
Background and Aims
Understanding the effect of meal composition on glucose excursion would be key in designing decision support systems (DSS) for type 1 diabetes (T1D) management. In fact, the amount of carbohydrates, lipids and proteins in a meal significantly affects postprandial gastric retention (GR), glucose absorption (GA) and insulin sensitivity (SI). Such variables can be estimated, in hospitalized setting, from plasma glucose and insulin data using the Oral Minimal Model (OMM, Dalla Man et al., 2002). Here, we developed a model to estimate those quantities in daily life conditions, using minimally invasive technologies (MI-OMM), and validated it against OMM.
Methods
Data collected from 47 patients with T1D (weight=77±10kg, age=41±13yr) in a closed loop clinical trial (Luijf et al., 2013) were used for model development and validation. Each participant underwent three randomized 23-hour visits (one open- and two closed-loop), during which plasma glucose and insulin were frequently collected, together with continuous glucose monitoring (CGM) and insulin pump (IP) data.
MI-OMM was identified from CGM and IP data using a Bayesian maximum a posteriori estimator, while OMM, identified from plasma glucose and insulin data, was used as reference.
Results
Both models fitted the data well and provided precise parameter estimates. Estimated GR, GA, and SI, obtained with the two methods, are compared in Figure 1.
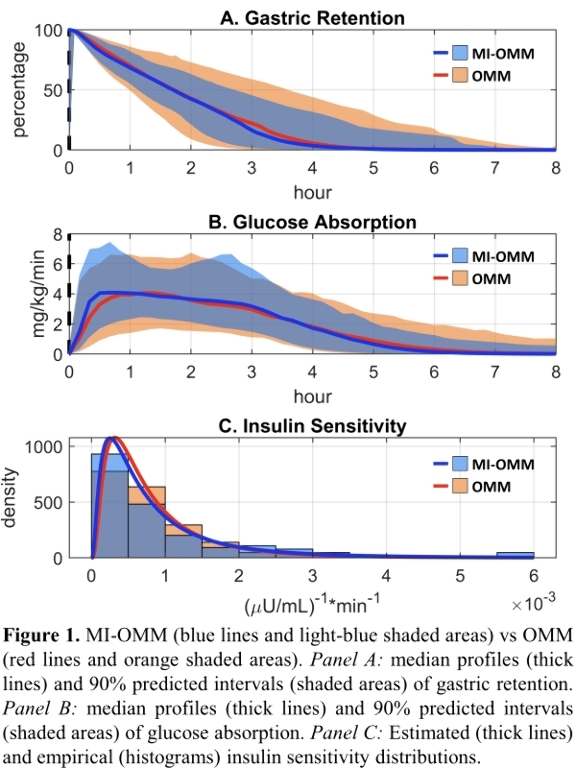
Conclusions
MI-OMM provided accurate estimates of GR, GA and SI using CGM and IP data. Therefore, it is usable to assess the effect of meal composition on those quantities in daily life conditions and potentially exploitable in DSS for T1D management.
EFFICACY OF THE INSULIN PEN SMART CAP INSULCLOCK® IN PEOPLE WITH NON-CONTROLLED TYPE 1 DIABETES MELLITUS (T1DM): A MULTICENTER, RANDOMIZED CLINICAL TRIAL
Abstract
Background and Aims
Insulclock®system includes an insulin pen smart cap and a digital platform to improve diabetes self-management, integrating insulin doses and CGM information. The study aimed to assess the efficacy of the Insulclock® system on improving glycemic control, treatment adherence, and quality of life in T1DM.
Methods
This multicenter, open-label, randomized, controlled trial in T1DM wearing a CGM device comprised a 4-week run-in period and a 6-week follow-up phase (participants were randomized to the active - used all functionalities, including alarm setting, data management and sharing with caregivers- or masked group). Glycemic control, glycemic variability, treatment adherence and the insulin treatment satisfaction questionnaire (ITSQ) were evaluated from the run-in to the follow-up period and compared between active and masked groups.
Results
Seventy-five participants were randomized, and 55 were analyzed (active group: 26; masked group: 29). The increase in time in range (TIR, primary outcome) was higher in the active vs the masked groups (+5.2% vs -0.8%; p = 0.016). The active group showed a higher reduction in mean glucose (-8.7 mg/dL; p = 0.024), eHbA1C (-0.31%; p = 0.039), time above range (TAR) 180 mg/dL (-5.5%; p = 0.018) and high blood glucose index (HBGI) (-1.4; p = 0.029). A higher increase in the insulin doses on time was observed in the active group (10.4% to 12.9%), masked group (12.2% to 8.7%)(p = 0.017). Most ITSQ items improved in both groups.

Conclusions
Insulclock®use was associated with improved glycemic control, glycemic variability, hyperglycemia risk, and insulin treatment adherence in people with uncontrolled type 1 diabetes.
ClinicalTrials.gov NCT04847778
ASSOCIATION BETWEEN CHANGE IN HBA1C AND PROFESSIONAL CGM USE IN ADULTS WITH TYPE 2 DIABETES ON NON-INSULIN THERAPIES–A REAL WORLD EVIDENCE STUDY
Abstract
Background and Aims
Previous studies have shown clinical benefits in patients who used professional Continuous Glucose Monitor (CGM). However, the effect of professional CGM use in non-insulin Type-2 Diabetes (T2D) patients having poor glycemic control in real world settings has not been studied. We examined the association between HbA1c and professional CGM in T2D patients with poor glycemic control using multiple non-insulin therapies.
Methods
This retrospective analysis used healthcare claims data from Optum® Clinformatics,® comprised of commercial and Medicare Advantage members between 01-January 2018 to 31-October 2020. T2D patients ≥ 18 years of age were identified using ICD-9/ICD-10 codes having an HbA1c between 7.8–10.5%, using ≥ 2 non-insulin therapies, with no prior CGM or professional CGM use, and 6-months of continuous enrollment pre and post index date. Index date was defined as acquisition of professional CGM identified through CPT codes 95250 and 95251. The outcome was mean HbA1c change between baseline and up to 6-months post-index date.
Results
Data from 15,474 eligible patients were assessed (Professional CGM users, n=677; Non-users, n=14,797). A significant decrease in mean HbA1c from baseline was observed for professional CGM users (-0.78) vs. non-users (-0.32), p <0.0001 (difference-in-differences estimate, -0.50; 95% CI,-0.61 to -0.39; p <0.0001).
Conclusions
Findings suggest T2D patients with poor glycemic control using multiple non-insulin therapies may benefit from professional CGM resulting in reduction in HbA1c over a 6-month period compared to usual care. Professional CGM can inform clinicians about their patients’ glycemic patterns and help to tailor diabetes management strategies for patients.
MY DIABETIC: SERIOUS GAME TO SUPPORT CHILDREN’S EDUCATION IN DIABETES MELLITUS I
Abstract
Background and Aims
Gaming applications that are used for purposes beyond entertainment, defined as serious games, with the intention to educate and resolve a problem, may be one timely method to promote healthy diabetes management behaviors within children affected by T1D.
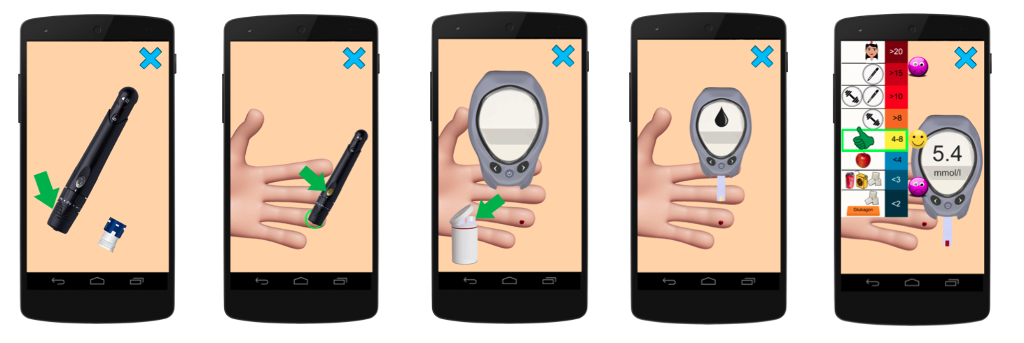
The aim of the serious game My-Diabetic is to teach players not only the relationship between food, insulin, and sports but also to pass on knowledge related to working with a glucometer insulin pen and more advanced technology like, injection of glucagon, measurement of ketoacidosis, continuous glucose measurement and insulin pump.
Methods
Supporting patient motivation (compliance, adherence) was achieved by a combination of several approaches as tailoring, observational learning, social and family support, decision-making practice, and rewards systems.

Results
The game was tested tested on 80 children (60 of diabetics). We met with positive response from children who tested the game and their parents. The game was also presented to 20 schoolmates of T!D's children who appreciated better understanding of the desease and opportunity to support more efficiently their friends in T1D compensation.
Conclusions
The game is especially suitable for newly diagnosed children because it acquaints them in a fun way with new terminology, they are able to try, for example, glycemic measurements in an interactive way. The game was also designed for children who cannot read yet because the game includes a guide (e.g. a female family doctor) that describes by her voice the main underlying principles behind the game. The game is available in Google Play and Apple Store markets.

The study was supported by the Research Centre for Informatics, grant number CZ.02.1.01/0.0/16_019/0000765
COST-EFFECTIVENESS OF A REAL-TIME CONTINUOUS GLUCOSE MONITORING SYSTEM VERSUS SELF-MONITORING OF BLOOD GLUCOSE IN TYPE 2 DIABETES PATIENTS ON INSULIN IN THE UNITED KINGDOM
Abstract
Background and Aims
A long-term health economic analysis was conducted to determine the cost-effectiveness of a real-time continuous glucose monitoring (rt-CGM) system versus self-monitoring of blood glucose (SMBG) in Type 2 diabetes (T2D) patients treated with insulin.
Methods
The IQVIA CORE diabetes model was used for the analysis. Clinical data were sourced from a US retrospective cohort study of adult T2D patients on insulin and adapted to the UK. The baseline mean age (SD) of the cohort was 61 years (13.2) and proportion of female 51%. Mean baseline HbA1c for the cohort was 8.3% (67 mmol/mol). Patients using rt-CGM were assumed to have a reduction in HbA1c of -0.56% based on the mean difference between groups after 12-months follow-up. A quality-of-life (QoL) benefit associated with reduced finger-stick testing was applied. The analysis was conducted from the UK National Health Service payer perspective over a lifetime horizon.
Results
The rt-CGM system was associated with an incremental gain of 0.76 quality-adjusted life years (QALYs) compared with SMBG (mean [SD] 8.44 [2.26] versus 7.68 [2.10] QALYs). Total mean [SD] lifetime costs were GBP 2,551 higher with rt-CGM (GBP 78,801 [45,749] versus 76,250 [49,564]), resulting in an incremental cost-effectiveness ratio of GBP 3,348 per QALY gained. Sensitivity analyses demonstrated findings were sensitive to changes in QoL, HbA1c, and younger patient cohorts.
Conclusions
For T2D patients on insulin, rt-CGM was associated with significant clinical outcomes and is a cost-effective management option relative to SMBG based on a willingness-to-pay threshold of GBP 20,000 per QALY gained.
