Welcome to the WSC 2022 Interactive Program
The congress will officially run on Singapore Standard Time (SGT/UTC+8)
To convert the congress times to your local time Click here
*Please note that all sessions in halls Summit 1, Summit 2 & Hall 406 will be live streamed in addition to the onsite presentation
ASK THE SPEAKER
Sessions in Halls 406, Summit 1 and Summit 2 have a Q&A component, through the congress App called “Ask the Speaker”
UNMASK - II STUDY (UTILITY OF NON CONTRAST MRI IN ACUTE STROKE) IMAGING RECLASSIFICATION OF ACUTE ISCHEMIC STROKE (UPDATED I-ASCOD PHENOTYPING)
Abstract
Background and Aims
Worldwide CT and CTA is the preferred imaging modality for acute stroke. However, MRI in acute stroke has been shown to be feasible and can even be cost-effective in developing countries such as India.
Imaging patterns can also help in the final reclassification of aetiopathogenesis and decide further medical management. We are MRI based tertiary stroke center performing non-contrast MRI in the emergency for treatment decisions regarding acute revascularisation and selected patients undergo modified CTA within 24-48 hours for further management such as secondary prevention.
We aim to re-classify stroke (updated ASCOD using imaging) based on MRI and modified CTA if available (I-ASCOD) in a dataset of ~1000 stroke codes.
Methods
In this study, we aim to describe our imaging experience of MRI based acute stroke workup over the last 3 years (2019 - 2022) and their imaging patterns based on MRI and correlate it with clinical details, labs, other available imaging (including modified CTA) and ancillary details at the time of discharge. Updated imaging-based ASCO-D phenotyping will be done.
Results
UNMASK-I: Published in WSC 2021, establishing the feasibility of MRI in acute stroke without significant delay compared to the currently recommended guidelines.
UNMASK- II Results pending
Conclusions
MRI can help in acute decision making as well as plan further management in the vast majority of stroke patients based on radiological patterns. The majority of centers around the world use combination of CTA and MRI during the hospitalization of acute stroke patients and updated I-ASCOD phenotyping can help overcome a few current shortcomings in stroke classification.
GLOBAL HYPERPERFUSION IS ASSOCIATED WITH A WORSE OUTCOME AMONG ACUTE ISCHEMIC STROKE PATIENTS UNDERWENT SUCCESSFUL ENDOVASCULAR TREATMENT
Abstract
Background and Aims
Patients with stroke may sometimes develop hyperperfusion after successful endovascular treatment (EVT). It is yet to be elucidated which factors affect post-EVT hyperperfusion and how hyperperfusion is associated with clinical outcome.
Methods
Consecutive patients who underwent EVT for anterior circulation occlusion and achieved successful recanalization (modified treatment in cerebral ischemia 2b–3) were reviewed. Hyperperfusion was categorized as follows based on post-EVT arterial spin labeling MRI: global hyperperfusion, increased cerebral blood flow (CBF) in ≥50% of previously occluded territory; focal hyperperfusion, increased CBF in <50% of previously occluded territory; and no hyperperfusion, no visible CBF increase. Factors associated with hyperperfusion were assessed and clinical outcome was compared among the hyperperfusion categories.
Results
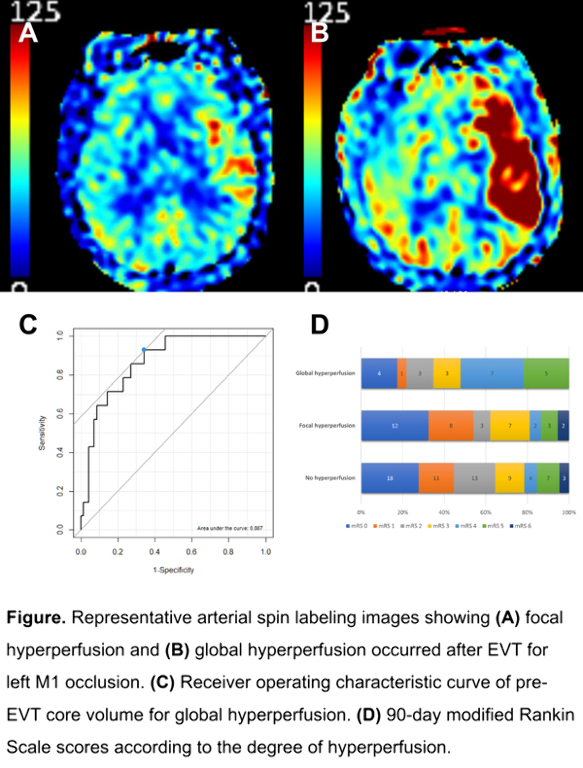
Among 125 eligible patients, 23 and 37 patients developed global and focal hyperperfusion, respectively. Compared with patients without hyperperfusion (n=65), global hyperperfusion group had worse neurologic severity and larger pre-EVT core. No significant difference was found between focal and no hyperperfusion groups. Pre-EVT core volume predicted global hyperperfusion with 92.9% sensitivity and 65.7% specificity (area under receiver operating characteristic curve, 0.867; 95% CI, 0.779–0.956). Global hyperperfusion group had worse 90-day outcome compared with focal hyperperfusion (modified Rankin Scale 0–2, 34.8% vs. 62.2%, p=0.072), and no hyperperfusion (34.8% vs. 64.6%, p=0.025) groups. Hemorrhagic transformation occurred similarly in the three groups.
Conclusions
Global hyperperfusion was associated with worse clinical outcome and tended to occur in patients with larger pre-EVT core. Future research is warranted to determine whether intervention such as blood pressure lowering improves outcomes in patients with global hyperperfusion.
DEEP LEARNING BASED LVO DETECTION ON CT ANGIOGRAPHY OF BRAIN
Abstract
Background and Aims
The early detection of anterior circulation large vessel occlusion (LVO) by computed tomography angiogram (CTA) is critical for treating acute ischemic stroke with mechanical thrombectomy.
We present a deep learning solution that detects Internal Carotid Artery (ICA) and M1/M2 Middle Cerebral Artery (MCA) occlusions on the maximum intensity projections (MIPs) of the brain's vascular territories (VTs).
Methods
Each CTA is preprocessed using a classifier which trims off the neck and keep only the brain.
A neurologist annotated the brain's left and right side of MCA and ICA territories on a single CTA. This is used as a reference to annotate VT maps on 942 CTAs.
These CTA scans were used to train and validate a deep learning based segmentation model which outputs brain VT masks and is aligned on corresponding CTA to get VT MIPs.
Deep learning based classification with segmentation models were trained on VT MIPs of 1083 MCA LVO positive scans, 840 ICA LVO positive scans, and 5142 LVO negative scans.
Results
Dice Similarity Coefficient (DSC) was adopted to validate the output of the segmentation model. VT outputs were validated on 232 CTAs with a DSC of 0.90.
| Validation Set | ||
| MCA LVO Detection | No. of positive scans | 445 |
| No. of negative scans | 2155 | |
| Sensitivity | 0.88 | |
| Specificity | 0.91 | |
| ICA LVO Detection | No. of positive scans | 360 |
| No. of negative scans | 2155 | |
| Sensitivity | 0.92 | |
| Specificity | 0.89 |
Conclusions
Even with the contrast contamination of veins, MIPs are not affected, and hence the deep learning model effectively and efficiently detects the ICA and MCA occlusions.


A DEEP LEARNING ANALYSIS OF STROKE ONSET TIME PREDICTION AND COMPARISON TO DWI-FLAIR MISMATCH
Abstract
Background and Aims
DWI-FLAIR mismatch rating is an established technique to estimate onset time of ischemic stroke in cases where it’s unknown. However, identifying subtleties in imaging is challenging even for experienced raters, especially in cases close to the 4,5 hrs threshold. Based on recent successes in medical imaging, Deep Learning (DL) might realize a promising way to augment human rating and improve accuracy.
Methods
We analyzed the performance of data-efficient Convolutional Neural Networks in estimating the onset time of ischemic stroke. We developed models on DWI and FLAIR imaging (N=489) and utilized unlabeled image data for pre-training (N=609). We tested a potential decision support scenario by augmenting human ratings with DL predictions in undeterminable cases. Additionally, we conducted an analysis to gain insights about DL predictions by post-hoc gradient-based explanations.
Results
Our DL approach improved the sensitivity of junior rating from 0.33 to 0.50, and senior rating from 0.43 to 0.48 while keeping specificity on a high level of 0.83. Junior rating gained more from augmentation by DL predictions than by senior rating due to notably high sensitivity of the model in undeterminable cases. Post-hoc explainability showed that our DL model successfully derived an association between stroke lesion and onset time without the need of explicit delineation.
Conclusions
We showed a potential use case where DL and post-hoc explanations could increase efficiency of stroke treatment selection in cases of patients with unknown onset times. Our approach does not depend on advance imaging or manual delineation, facilitating acceleration of acute decision making and aiding inexperienced raters.
ARTIFICIAL INTELLIGENCE FOR DECISION SUPPORT IN ACUTE ISCHEMIC STROKE CARE: A SYSTEMATIC REVIEW
Abstract
Background and Aims
In recent decades, several biomarkers have emerged from prospective trials facilitating the time-sensitive decision making in ischemic stroke. Despite general successes, they lack personalization, which has prompted attempts to revolutionize stroke diagnosis and treatment decision support through artificial intelligence (AI) methods. We created a systematic review of decision support systems using AI for acute ischemic stroke care that aims to provide an overview of the level of methodological robustness and standardization within the field.
Methods
We included full-text publications that propose an AI method for decision support in adult patients with acute ischemic stroke in the acute setting. Our primary objective was to describe the data, methodology, performance and outcomes used in those systems. A total of 139 studies met our inclusion criteria. Among these, 65 were included for full extraction while 74 studies were identified as proposing a method for automated stroke scoring only.
Results
There was a high degree of heterogeneity in the data sources used, methods applied, and reporting practices that were followed in our sample. We found a low level of adherence to the MINIMAR checklist.
Conclusions
There has been undeniable progress in the performance of AI models, however our results suggest significant potential validity threats, dissonance in reporting practices and challenges to clinical translation across the studies we reviewed. We outline practical recommendations for clinicians, researchers, journals and funding agencies, who all have a role to play in safeguarding the quality of research and in enabling the exploitation of the promise of AI in acute ischemic stroke care.
AI-BASED PREDICTION OF IMMINENT PRIMARY STROKE ON CLAIMS DATA ENABLES ACCURATE PATIENT STRATIFICATION
Abstract
Background and Aims
Direct treatment and follow-up costs due to permanent disability after an ischemic stroke are increasing fast. Current approaches fail to identify high-risk profiles of imminent stroke and focus on mid- to long-term risk assessment, crucially impeding individualized preventative action. Claims data may support the development of new risk prediction paradigms for personalized management of disease.
Methods
We developed a data-driven paradigm to predict personalized risk of imminent primary ischemic stroke based on social health insurance data from northeast Germany. Stroke events were defined by the presence of an ischemic stroke ICD-10 diagnosis within the available insurance period. Controls (n=150,091) and strokes (n=53,047) were matched by age and insurance length, resulting in a generally aged, high-risk study population. We trained traditional and Machine Learning (ML) classifiers to predict the overall likelihood of a primary event based on 55 features including demographic parameters, ICD-10 diagnosis of diseases and dependence on care. Binary ICD-10 features were translated into temporal duration of diagnoses by counting days since the first appearance of disease in the patients’ records.
Results
The best ML model, Tree-boosting, yielded excellent performance with an area under the receiver operating characteristics curve of 0.91, sensitivity of 0.84 and specificity of 0.81. Long duration of hypertension, dyslipidemia and diabetes type-2 were most influential for predicting stroke according to feature importance ranking.
Conclusions
Our proposed data-driven ML approach provides a highly promising direction for improved, personalized prevention and management of imminent stroke, while the developed models offer direct applicability for risk stratification in northeast Germany.
