Welcome to the WSC 2021 Interactive Program
The congress will officially run on Central European Summer Time (CEST/GMT+2)
To convert the congress times to your local time Click Here
The viewing of sessions cannot be accessed from this conference calendar.
All sessions are accessible via the Main Lobby on the Virtual Platform.
 - WSC TV
- WSC TV  - Live Session
- Live Session  - Pre-Recorded Session with Live Q&A
- Pre-Recorded Session with Live Q&A  - On Demand Session (watch anytime)
- On Demand Session (watch anytime) ![]() - Session with Voting
- Session with Voting
COLLECTIVE AND MULTIMODAL PHYSICAL ACTIVITY IMPROVED ACTIVITY LIMITATIONS FOR STROKE SURVIVORS IN LOW INCOME SETTINGS: FEASIBILITY AND EFFICACY OF A RANDOMIZED CONTROLLED TRIAL WITH CROSS-OVER
Abstract
Background and Aims
Post-stroke disability leads victims to physical inactivity and activity limitation. Although several protocols of physical activity have been shown to be effective for poststroke people, their modalities were trial dependent, sometimes expensive and less accessible in low income settings. To investigate the feasibility and efficacy of a Circuit walking, Balance, Cycling and strengthening trainings (CBCS) trial on activity limitation in people with chronic stroke.
Methods
Forty-six community-dwelling chronic stroke individuals, no longer undergoing rehabilitation, were randomly assigned to either experimental group (n = 23, CBCS trainings; 2 hours sessions, 3/weeks for 12 weeks) or the control group (n = 23, passive socio-cultural activities; same duration and intensity as experimental group). Afterwards, both groups were crossed over and trained for the same duration and intensity. Feasibility was assessed by retention, adherence rate and safety while efficacy was assessed by the ACTIVLIM-Stroke scale (activity limitation) and 6MWT (walking endurance). Outcomes were measured at baseline, after intervention (12 weeks), at 6 months (after cross-over) and at follow up (3 months).
Results
The retention rate was 100% while the adherence was 93%. Minor adverse events occurred in 10% of cases during the first week. A two (groups) × four (test sessions) analysis of variance indicated significant improvements of activity limitations (ACTIVLIM-stroke, p < .001) and walking endurance (6MWT, p<.001) in the experimental group compared to control. The effects obtained remained improved at follow-up.
Conclusions
Collective and combined physical activity was feasible and safe. It improved functional independence (activity limitation) and walking endurance in chronic stroke survivors.
VAGUS NERVE STIMULATION PAIRED WITH UPPER LIMB REHABILITATION AFTER CHRONIC STROKE: CROSS-OVER RESULTS FROM THE VNS-REHAB PIVOTAL TRIAL.
Abstract
Background and Aims
In the VNS-Rehab trial, active Vagus Nerve Stimulation (active-VNS) paired with rehabilitation led to a greater reduction in upper limb impairment compared to sham-VNS paired with rehabilitation. We report here results from participants who received sham-VNS paired with rehabilitation that crossed over to receive active-VNS paired with rehabilitation.
Methods
Forty-nine participants received 6 weeks of in-clinic sham-VNS paired with rehabilitation followed by a 90-day sham-VNS home exercise program. Participants then received 6 weeks of in-clinic active-VNS paired with rehabilitation followed by a 90-day active-VNS home exercise program. Upper limb impairment (Fugl-Meyer Upper Extremity score (FMA-UE)) was assessed at baseline, after the sham-VNS phase, after the 6-weeks of in-clinic active-VNS paired with rehabilitation and after the 90-day active-VNS home exercise program. Values are means[standard error]. Significance difference was set at p<0.05. A clinically meaningful response was defined as a >6 point change in FMA-UE score.
Results
No related or unexpected adverse or serious adverse events were reported. FMA-UE score increased from 35.7[1.1] at baseline by +3.1[0.8] following the sham-VNS phase (p<0.0002). FMA-UE score significantly increased further by +2.8[0.5] (p<0.0001) after 6-weeks of in-clinic active-VNS and by +2.4[0.7] (p<0.002) following the 90 day active-VNS home exercise program. The overall increase from baseline to the end of the active-VNS phase was +5.9[0.9] (p<0.001). A clinically meaningful response occurred in 24% of participants following the sham-VNS phase but increased to 44% following the active-VNS phase.
Conclusions
On average, participants who initially received sham-VNS paired with rehabilitation achieved a further reduction in impairment following active-VNS paired with rehabilitation.
NOVEL MACHINE-LEARNING ANALYSIS TO PREDICT OUTCOMES DURING INPATIENT REHABILITATION
Abstract
Background and Aims
We used novel machine learning (ML) techniques to predict change on the Functional Independence Measure (FIM) and each of its subcategories from inpatient rehab admission to discharge.
Methods
We propose a novel ML model, Zero-inflated Random Forest (ZiRF), to predict changes in FIM scores for each FIM subcategory from admission to discharge. We compared the proposed model with statistical learning and deep learning (DL) algorithms. Compared with statistical methods, ZiRF captures complex non-linear, interactive effects among predictors, mitigates the zero-inflation problem, and provides interpretable results compared with black-box DL methods. Mean absolute error (MAE) was used to estimate the prediction error across the 18 FIM score subcategories. The MAE per subject measures the prediction accuracy (lower MAE shows superior prediction accuracy).
Results
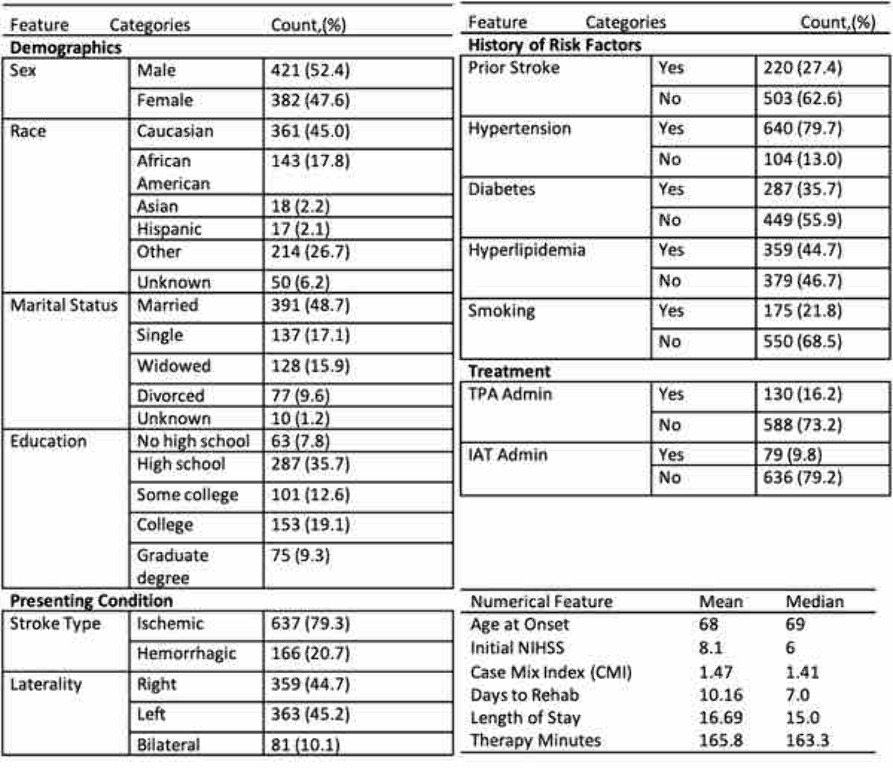
Fig 1 shows the demographics and clinical features of the study population of over 800 patients. ZiRF not only demonstrates superior predictive accuracy (MAE: 15.148) compared to linear regression (16.210), XGBoost (16.377), and random forest (21.753) but also generates interpretable inferences by identifying influential variables. The effect of each variable is represented by its Lasso coefficient obtained by fitting a cross-valued Lasso regression on each FIM score category. Among the top five predictors, age (OR = -1.7), Case Mixing Index (CMI) (OR = 1.5), length of stay in rehabilitation (OR = 1.2), duration of therapy (OR = 1.1), and Initial NIHSS score (OR = 0.75) are the most influential on functional outcome.
Conclusions
We present a novel model using ML to predict functional improvement for stroke patients receiving inpatient rehabilitation.
ENVIRONMENTAL ENRICHMENT, REHABILITATION OUTCOME AND THE PANDEMIC: ESTABLISHING A CONNECTION
Abstract
Background and Aims
Environmental Enrichment (EE) for stroke patients encompass a dynamic environment which encourages socialization, sensori-motor activities and cognitive stimulation beyond direct therapy time. Pandemic impact of physical distancing potentially affects socialization, an important EE element. Due to pandemic-appropriate measures in hospital-setting, patients narrated reduced socialization opportunity caused by restricted communal and group activities. The aim is to establish the inpatient stroke rehabilitation outcome trend based on pre/post-EE implementation phases; prior and during pandemic.
Methods
Environmental Enrichment (EE) initiatives were implemented in structured stages based on the Exploration-Planning-Implementation-Sustainment (EPIS) Framework. EE Exploration-Planning Phase occurred in 2018. EE Implementation Phase (2019-2020) focus on multi-faceted activities using various apparatus, incorporating self-directed tasks and communal sessions with caregivers' involvement. A chronological timeline-matching approach was used to match EE implementation initiatives and rehabilitation impact indices comprising of Absolute Functional Gain (AFG) and Rehabilitation Efficiency Index (REI) utilizing Modified Barthel Index. Trending was compared for 2018 (Pre-EE Implementation/Pre-Pandemic), 2019 (EE Implementation/Pre-Pandemic) and 2020 (EE-Implementation/Pandemic) phases.
Results
Compared to 2018, there was incremental improvement in AFG and REI in 2019 (EE-Implementation/Pre-Pandemic). When compared to 2019, marginal reduction of AFG and REI was noted in 2020 (EE-Implementation/ Pandemic). Median (IQR) for AFG were 17.5(11-30), 22(13-35), 20 (9-33.5) for 2018, 2019 and 2020 respectively. Median (IQR) for REI were 0.8 (0.5-1.3), 1.1 (0.5-1.5), 1.0 (0.5-1.3) for 2018, 2019, 2020 respectively.
Conclusions
Environmental enrichment potentially promotes post-stroke recovery and improve stroke rehabilitation outcome. Although pandemic-appropriate measures may affect EE socialization component, an active effort is important to implement and embed EE initiatives in the inpatient rehabilitation setting.
RISK AND ASSOCIATED FACTORS FOR HEMIPLEGIC SHOULDER PAIN IN PEOPLE WITH STROKE: A SYSTEMATIC LITERATURE REVIEW
Abstract
Background and Aims
Hemiplegic shoulder pain (HSP) is reported in up to 47% of people with stroke. Since the development of the national guidelines for stroke, the management of HSP has evolved. The aim of this systematic literature review was to explore the risk and associated factors for HSP for studies published in the last 15 years.
Methods
A systematic online search was conducted of CINAHL, AMED, MEDLINE and the Cochrane Library databases using appropriate keywords. The search was supplemented by hand searching of relevant journals and citation tracking of the retrieved papers. All primary studies published in English language fulfilling the review’s inclusion criteria were included. Five reviewers extracted the data and independently appraised the methodological quality of the selected studies. Any discrepancies were resolved following discussions.
Results
Of the 50 articles that were identified, 21 studies met the criteria. The common risk factors for HSP were: Poor motor function (odds ratio (OR) ranging from 0.58-3.19; 95% confidence interval (CI), 1.1-7.7); glenohumeral subluxation (OR ranging from 2.48-3.5, 95% CI 1.38-9.37) and reduced range of movement at the shoulder (OR 0.14-4.46, 95% CI 0.99-64).
Conclusions
Despite methodological flaws, complete loss of motor function in the affected arm and glenohumeral subluxation have been recognized as significant risk factors for HSP. Further rigorously designed research studies are required. The best way to prevent HSP, based upon current evidence, is to strengthen shoulder rotator cuff muscles and improve motor control around the shoulder region. In addition, education to both the caregivers and patients is critical.
AUTOMATION OF FUGL-MEYR ASSESSMENT
Abstract
Background and Aims
Majority of Stroke patients are afflicted with Hemiparesis, characterized by weakness and partial loss of function in one side of the body. To monitor motor recovery post Stroke, the Fugl-Meyer assessment (FMA) is the most popular index for evaluating upper extremity motor function in stroke patients. In order to overcome inter-physician variability in scores and establish more frequent assessments at low-cost, we propose to automate FMA using the power of Artificial Intelligence.
Methods
The system comprises of a software which can be deployed on a medium-end computer that captures a video of the patient performing the prompted movement using a webcam, detects the joints with the help of Google’s Mediapipe pose estimation model, processes the localized joints frame by frame using a rule-based classifier, and returns the score for the corresponding movement.
Results
For efficient extraction of features, the subject is to be seated 2m away from the camera and at an orientation of either 0 or 45 degrees depending on the class of movement. The proposed system has been able to process the sequentially detected joints and extract the desired features for scoring of 24 movements of Upper-extremity.
Conclusions
The automated, cost-efficient framework aids the patient to monitor their progress more frequently from their homes. In addition to the qualitative FMA scores, the extracted features such as movement time, velocity, range of motion provides a quantitative estimate of improvement over time. Thus, the Physician can alter the course of rehabilitation by monitoring the performance and needs of the patient flexibly and remotely.
A NOVEL TOOL FOR QUANTITATIVE ASSESSMENT OF LOWER LIMB PROPRIOCEPTION: A DEMONSTRATION WITH A STROKE SURVIVOR
Abstract
Background and Aims
Stroke is a common cause for proprioceptive impairments. Current clinical proprioception assessment methods are subjective and inconsistent. To address these limitations, we developed a quantitative assessment tool of lower limb proprioception.
Methods
We developed a tool using magnetic position trackers placed on the toes of the participants while laying on their sides. We evaluated the affected (A) and unaffected (U) limbs with ipsilateral (UU, AA) and contralateral (UA, AU) position matching conditions. We compared young adults and stroke survivors' mean-absolute-error (MAE), bias, and mean-variable-error (MVE). We defined a threshold of 90% of cumulative distribution in two targets to detect impairment and compared the conditions to isolate potential proprioceptive, motor or cognitive impairments. For example, impaired AU and AA would indicate a likely proprioceptive impairment of the affected limb.
Results
Conditions AU, AA and UU were impaired, suggesting potential proprioceptive and motor impairments of the affected and unaffected limbs, respectively, and a spatial memory impairment.
Conclusions
We demonstrated the tool's usage with a stroke survivor (Fig 1), who displayed potential impairments. Without confounding effects of fatigue, the patient likely suffered from proprioceptive and motor impairments in the affected and unaffected limbs, respectively.

Acknowledgments: Special acknowledgments to the Israeli Ministry of Science and Technology and the Multidisciplinary scholarship of Ben-Gurion University of the Negev for funding and Noy Goldhamer for assistance.
TASK-SPECIFIC EFFECTS ON BRAIN ACTIVITY AFTER STROKE
Abstract
Background and Aims
Evidence supports cortical reorganization in sensorimotor areas induced by constraint-induced movement therapy (CIMT). However, little is known about how task specificity during training affects cortical reorganization. This provoked us to retrospectively analyze an imaging dataset from chronic stroke survivors before and after participation in the signature CIMT protocol. This retrospective analysis aims to evaluate the functional brain activation changes during a precision and a power grasp task in chronic stroke survivors who received two-weeks of CIMT compared to a control group.
Methods
Before and after a 2-week period, 14 chronic stroke survivors, randomized to CIMT (n=8) or non-CIMT (n=6), underwent functional MRI (fMRI). During scan runs, a precision and a power grasp tasks were performed. Pre to post changes in laterality index (LI) were compared by group and task, using a multiple linear regression, for two predetermined motor regions of interest: dorsal premotor cortex (PMd) and primary motor cortex (MI).
Results
Compared to the non-CIMT control group, two weeks of task specific training produced a greater shift in functional activation toward the dorsal premotor region of the lesioned hemisphere during the precision grasp task in the CIMT group (F(4,20)=4.65, p=0.012, adj. R2=32.3%). However, no changes in LI were observed in MI for either task or group (F(4,20)=1.05, p=0.389, adj. R2=0.72%).
Conclusions
Intense progressive precision grasp training drives recovery-supportive functional plasticity in the dorsal premotor cortex of the lesioned hemisphere. The results provide strong evidence for the principle of specificity and intensity of experience-dependent plasticity in stroke survivors.
RESPIRATORY FUNCTION AND FUNCTIONAL CAPACITY IN CHRONIC STROKE PATIENTS
Abstract
Background and Aims
Background: In addition to sensory-motor deficits, post-stroke individuals usually show impaired lung function, which can lead to a reduction in physical activity and/or physical fitness. Aim: To evaluate levels of physical activity as measured with the self-reported HAP (using the Adjusted Activity Score) and pulmonary function in stroke survivors.
Methods
Fifty post-stroke individuals in the chronic phase, with a mean age of 56,98 ± 13,23 years and BMI of 26,85 ± 4,86 Kg/m2 were invited to answer the Human Activity Profile ( HAP) questionnaire ,used to evaluate the level of physical activity according to increasing energy expenditure. Subjects also performed lung function test. Forced expiratory volume in one second (FEV1) and forced vital capacity (FVC) using a spirometer were measured according to the guideline from American Thoracic Society.
Results
Self-reports of physical activity according to the HAP classification revealed that 58.3% of the individuals were inactive, 29.1% moderately active and active. The mean values obtained for the FEV1 were 2,02 ± 0,69 and 2,83± 0,38, and FVC were 2,39 ± 0,79 and 3,35 ± 0,64 for the inactive, and moderately and active groups, respectively (p< 0.01).
Conclusions
The present study identified that the sample of patients who were in the chronic phase of the stroke, have reduced changes in respiratory capacity and levels of physical activity, which are correlated. The impact and importance of physiotherapeutic assessments and interventions involving the respiratory system as part of stroke rehabilitation at this stage is observed, in order to promote quality of life.

