P. Padilla (Des Plaines, US)
American Hip Institute Research FoundationPresenter Of 7 Presentations
12.3.10 - Application of Deep Learning Models to Predict Achievement of PASS at Minimum 2-Year Follow-Up After Primary Hip Arthroscopy
Abstract
Purpose
To identify predictive factors for achieving PASS in patients undergoing primary hip arthroscopy and labral repair for femoroacetabular impingement syndrome (FAIS) and labral tears.
Methods and Materials
Data were prospectively collected and retrospectively reviewed on all patients undergoing primary hip arthroscopy and labral repair for femoroacetabular impingement syndrome (FAIS) and labral tears between July 2015 and May 2019. The primary outcome was achievement of PASS based on an anchor-question at minimum 2-year follow up. A Multilayer Perceptron Artificial Neural Network (MLP-ANN), Extreme Gradient Boosting (XGBoost), and logistic regression models were trained on an independent testing set of patients to identify significant predictors.
Results
A total of 343 patients were included with 263/343 (76.7%) achieving the PASS threshold at minimum 2-year follow-up. A combination of 4 variables optimized model performance: capsular management (repair vs unrepair of interportal capsulotomy), labral size (<4 mm or ≥4 mm in the anterosuperior quadrant), age (years), and body mass index (BMI). The MLP-ANN model demonstrated the best accuracy (R2 = 78.1%) followed by the logistic regression (R2 = 71.8%) and XGBoost (R2 = 71.3%). The logistic regression found labral size ≥ 4mm to be the only statistically significant variable for predicting achievement of PASS (Odds Ratio: 2.444, P = 0.026). Patients with labral size ≥ 4mm achieved PASS at a rate of 78.7%, and patients with labral size < 4mm achieved PASS at a rate of 59.4% (P = 0.0244).
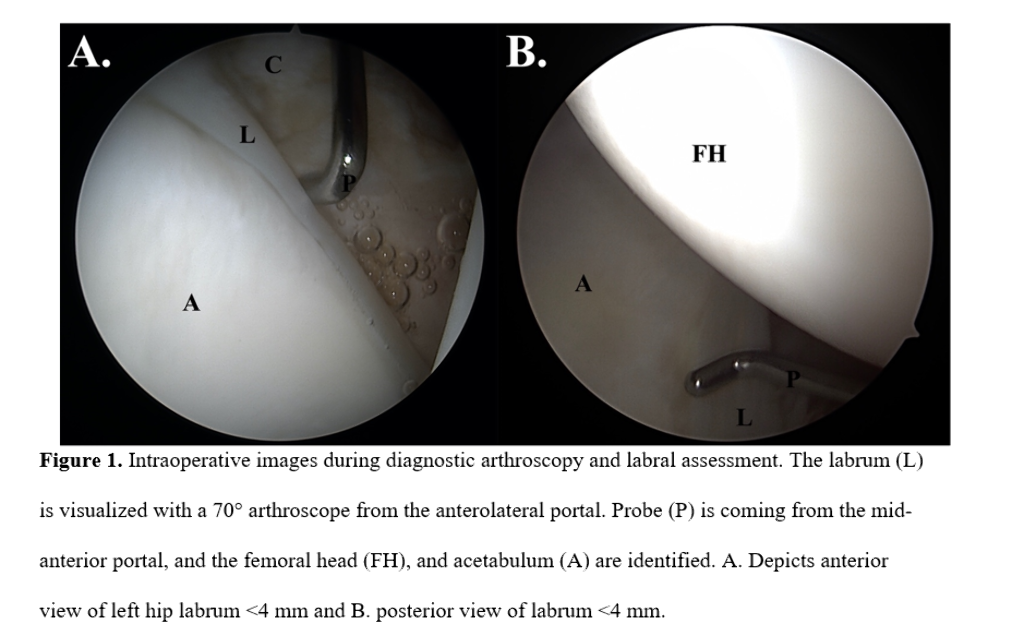
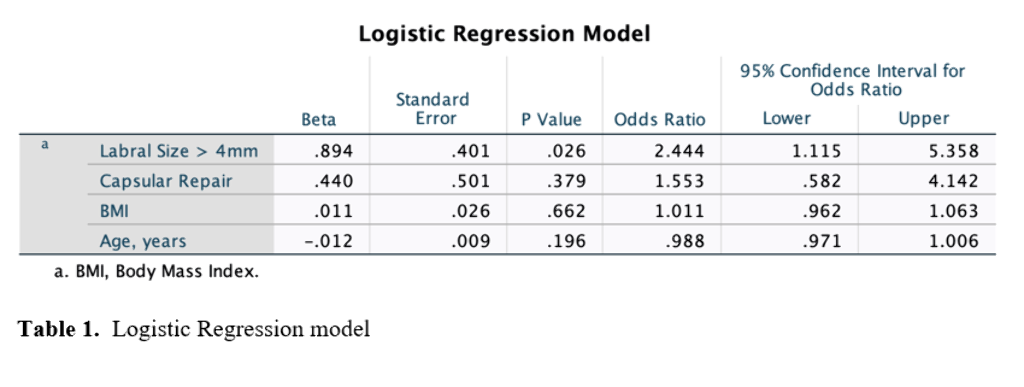
Conclusion
Labral size, capsular management, age, and BMI were found to be significant predictors of achieving PASS at minimum 2-year follow-up in patients undergoing primary hip arthroscopy and labral repair. Labral size ≥ 4 mm was the most statistically significant factor in favor of achieving PASS in this patient population.
24.2.2 - Labral Tear Management in Patients Aged 40 Years and Older Undergoing Primary Hip Arthroscopy
Abstract
Purpose
To report minimum two-year patient-reported outcome (PRO) scores, survivorship, and secondary surgeries, in patients aged ≥ 40 years who underwent primary hip arthroscopy with labral reconstruction compared to a propensity-matched primary labral repair group.
Methods and Materials
Data were prospectively collected and retrospectively reviewed for patients who underwent a primary hip arthroscopy for femoroacetabular impingement syndrome from January 2014 to June 2018. Patients aged ≥ 40 years who underwent a labral reconstruction or a labral repair and had preoperative and minimum two-year PROs for the modified Harris Hip Score (mHHS), Non-arthritic Hip Score (NAHS), and visual analog scale (VAS) for pain were included. Patients with prior ipsilateral hip conditions and surgery, Tonnis grade > 1, hip dysplasia, or worker’s compensation status were excluded. Patients in the reconstruction group were propensity-matched 1:2 to patients in the repair group based on age, sex, and body mass index. Secondary surgeries and the achievement of the minimal clinically importance difference (MCID), patient acceptable symptomatic state (PASS), and maximum outcome improvement (MOI) were recorded.
Results
Fifty-three and 106 hips were included in the labral reconstruction and repair groups, respectively. The average follow-up time was 37.6 months. The average age for the reconstruction and repair groups were 48.01 ± 5.4 years and 48.61 ± 6.0 years, respectively. Both groups achieved significant improvements in all PROs with similar achievements of MCID, PASS, and MOI. Both groups showed comparable secondary surgeries rates.
Conclusion
Patients aged 40 years and older who received primary labral repair and primary labral reconstruction, achieved similar significant improvements in all PROs, VAS pain, and patient satisfaction at minimum two-year follow-up, with comparable rates of secondary surgeries and achieving MCID, PASS, and MOI. Based on these findings, labral repair remains the gold standard treatment for viable labrum in this population group, while reconstruction is a useful alternative for irreparable labrum.
24.2.4 - Minimum 10-Year Follow-Up Outcomes and Survivorship Following Primary Hip Arthroscopy With Acetabular Microfracture
Abstract
Purpose
To report minimum 10-year follow-up patient-reported outcomes (PROS) in patients following primary hip arthroscopy in the setting of femoroacetabular impingement syndrome with acetabular microfracture, and 2) to report the survivorship, defined as non-conversion to total hip arthroplasty (THA) within the same period.
Methods and Materials
Data was prospectively collected and retrospectively analyzed on all patients who underwent a primary hip arthroscopy and received an acetabular microfracture between May 2009 and January 2011 and included in this study. Eligible patients completed preoperative patient-reported outcomes (PROS) questionnaires for the Modified Harris Hip Score (mHHS), Nonarthritic Hip Score (NAHS), the Hip Outcome Score – Sport-Specific Subscale (HOS-SSS), and the visual analog scale (VAS) for pain. Patients were excluded from this study if they had previous ipsilateral hip surgery, Tönnis osteoarthritis grade > 1, or previous hip conditions. The demographics, intraoperative findings, surgical procedures, PROs, and secondary surgeries were analyzed.
Results
25 hips were included in the study. There were 10 hips (43.5%) from males and 13 hips (56.5%) from females. The average patient age at the time of surgery was 43.3 years ± 11.1 (25.5 – 65.6), and the follow-up time was 123.9 ± 2.3 months (120.0 – 128.1). All patients on average experienced significantly improvement between preoperative and postoperative PROs in the mHHS (P < 0.001), NAHS (P < 0.001), HOS-SSS (P = 0.004), and VAS for pain (P < 0.001). In total, 65.2% of the patients did not require conversion to THA.
Conclusion
Significant improvement in all PROs and survivorship over 65% were obtained following acetabular microfracture for the management of focal and full-thickness cartilage lesions in primary hip arthroscopy. Based on the results, acetabular microfracture seems to be a feasible and valid alternative for severe and focal cartilage defects.
24.2.5 - Athletes Given Capsular Repair Have Successful Outcomes: A Propensity-Matched Analysis With Minimum 2-Year Follow-Up
- A. Jimenez (Des Plaines, US)
- B. Domb (Des Plaines, US)
- M. Lee (Des Plaines, US)
- D. Radwanski (Des Plaines, US)
- J. Owens (Des Plaines, US)
- B. Saks (Des Plaines, US)
- D. Maldonado (Des Plaines, US)
- A. Lall (Des Plaines, US)
- T. Harris (Des Plaines, US)
- P. Sabetian (Des Plaines, US)
- P. Padilla (Des Plaines, US)
Abstract
Purpose
To compare minimum 2-year patient reported outcome scores (PROs) and return to sport (RTS) between high-level athletes who undergo primary hip arthroscopy with a capsular repair and high-level athletes undergoing primary hip arthroscopy with an unrepaired interportal capsulotomy.
Methods and Materials
Data on all professional, collegiate, and high-school athletes who underwent primary hip arthroscopy between February 2012 and December 2018 were collected. Athletes were divided into 2 groups based on whether they received a capsular repair (R) or an unrepaired interportal capsulotomy (UR). Minimum 2-year PROs were collected for the Nonarthritic Hip Score (NAHS), Hip Outcome Score-Sports Specific Subscale (HOS-SSS), visual analog scale (VAS) for pain, and RTS status. R athletes were propensity-score matched to UR athletes for comparison.
Results
A total of 53 UR athletes (53 hips) with an average follow-up time of 36.5 ± 10.2 months were propensity-score matched to 84 R athletes (84 hips) with an average follow-up time of 41.3 ± 9.4 months. R athletes demonstrated significantly greater magnitude of improvement from preoperative to minimum 2-year postoperative scores for NAHS (P = 0.01), HOS-SSS (P = 0.001), and VAS (P = 0.01). Further, R athletes demonstrated significantly higher rates of achieving MCID for NAHS (73.8% vs 54.7%, P = 0.034) and HOS-SSS (65.5% vs 37.7%, P = 0.003) compared to UR athletes. RTS rates were higher in R athletes compared to the UR athletes, but this did not reach statistical significance (80.6% vs 65.9%, P = 0.170).


Conclusion
High-level athletes who undergo primary hip arthroscopy and capsular repair demonstrated significantly greater magnitude of improvement in PROs (NAHS, HOS-SSS, and VAS) compared to a control group athletes with an unrepaired interportal capsulotomy.
P020 - Primary Segmental Labral Reconstruction for Irreparable Labral Tears in the Hip: Minimum Five-Year Outcomes
- B. Domb (Des Plaines, US)
- D. Maldonado (Des Plaines, US)
- C. Kyin (Des Plaines, US)
- J. Simpson (Des Plaines, US)
- S. Annin (Des Plaines, US)
- A. Jimenez (Des Plaines, US)
- B. Saks (Des Plaines, US)
- A. Lall (Des Plaines, US)
- T. Harris (Des Plaines, US)
- P. Padilla (Des Plaines, US)
- P. Sabetian (Des Plaines, US)
Abstract
Purpose
1) To evaluate minimum 5-year patient-reported outcome scores (PROs) in patients who underwent primary SLR with hamstring graft, in the setting of femoroacetabular impingement syndrome (FAIS) and irreparable labral tears, and 2) to compare the outcomes of hamstring autograft vs. allograft in a subanalysis using propensity-matched groups.
Methods and Materials
Prospectively collected data were retrospectively reviewed for patients who underwent primary hip arthroscopy from September 2010 to November 2015. Patients were included if they underwent SLR using hamstring autograft or allograft and had preoperative and minimum 5-year PROs. Exclusion criteria were previous ipsilateral hip surgery/conditions, dysplasia, or Tönnis grade > 1. Patients with autograft SLR were propensity-matched 1:1 based on age, gender, and body mass index (BMI) to patients who underwent SLR using hamstring allograft. The minimal clinically important difference (MCID), and patient acceptable symptomatic state (PASS) were calculated.
Results
48 hips were eligible to be included in this study, and 41 hips (85.4%) had minimum 5-year follow-up reporting significant improvement in all PROs. Fifteen of the 41 included patients underwent a SLR with a hamstring autograft and were matched to 15 patients with labral reconstruction using allograft hamstring. Groups were similar for gender (P >.999), age (P = .775), and BMI (P = .486). The average follow-up time was 80.8 ± 25.5 and 66.1 ± 8.3 months (P = .223) for the autograft and the allograft groups, respectively. Baseline PROs, preoperative radiographic measurements, surgical findings and intra-operative procedures were similar. The groups achieved significant and comparable improvement for all PROs (P < .0001), satisfaction (P = .187), and rate of achieving the MCID and PASS.
Conclusion
At minimum 5-year follow-up, patients who underwent primary arthroscopic SLR, in the context of FAIS and irreparable labra, reported significant improvement and comparable postoperative scores for PROs, patient satisfaction, MCID, and PASS using either autograft or allograft hamstrings.
P085 - Non-Arthritic Hip Pathology Patterns According to Gender, Femoroacetabular Impingement Morphology and Generalized Ligamentous Laxity
- B. Domb (Des Plaines, US)
- D. Maldonado (Des Plaines, US)
- V. Ortiz-Declet (Westwood, US)
- L. Yuen (Hanover, US)
- S. Annin (Des Plaines, US)
- C. Kyin (Des Plaines, US)
- A. Jimenez (Des Plaines, US)
- A. Lall (Des Plaines, US)
- P. Sabetian (Des Plaines, US)
- T. Harris (Des Plaines, US)
- P. Padilla (Des Plaines, US)
Abstract
Purpose
To identify hip pathology patterns according to gender, alpha angle deformity and generalized ligamentous laxity (GLL) in a non-arthritic patient population following primary hip arthroscopy for femoroacetabular impingement syndrome.
Methods and Materials
Patients who underwent primary hip arthroscopy between February 2008 and February 2017 were included and separated into males and females for initial analysis. The demographics, radiographic findings, intraoperative findings, and surgical procedures were then compared. A threshold of one standard deviation above the mean alpha angle in the male group was used to create two sub-groups. For females, GLL based on a Beighton’s score ≥4 was used to divide the group.
Results
A total of 2701 hips were included. Of those, 994 hips were in the male group and 1707 hips in the female group. Mean age was 36.6 years±13.8 and 37.1 years±15.0 for the male and female groups, respectively. The male group had a higher average alpha angle when compared to females [65.9°±11.9 vs 58.4°±10.8 (P<0.001)]. GLL was more common in females than males (P< 0.001). The male group had a higher proportion of acetabular Outerbridge grade 3 and 4 lesions compared to the female group (P<0.0001). Males in the alpha angle ≥78° sub-group reported higher rates of acetabular Outerbridge grade 4 damage than males in the <78° one (P<0.0001). Mean lateral center-edge angle was lower in the Beighton ≥4 female sub-group [23.7°±4.2 versus 31.3°±5.8 (P<0.0001)].
Conclusion
Two different patterns of hip pathologies were found to be related to gender. On average, male patients had higher alpha angles and increased acetabular chondral damage when compared to the females. A larger cam-type anatomy was associated with more severe acetabular chondral damage in males. In the female group, the incidence of features of hip instability such as GLL were significantly higher than in the male group.
P163 - Application of Deep Learning Models to Predict the Need for Revision Surgery in High-Level Athletes
Abstract
Purpose
To identify predictive factors for undergoing revision surgery in a cohort of high-level athletes undergoing primary hip arthroscopy for femoroacetabular impingement syndrome (FAIS).
Methods and Materials
Data were reviewed on all patients undergoing primary hip arthroscopy for femoroacetabular impingement syndrome (FAIS) between July 2008 and May 2019. Patients were included if they competed in professional, collegiate, and high school sports and had minimum 2-year follow-up for the Hip Outcome Score – Sport Specific Subscale (HOS-SSS). The primary outcome was undergoing arthroscopic revision surgery. Recursive feature selection was used to identify predictive variables from an initial pool of 27 features. A Multilayer Perceptron Artificial Neural Network (MLP-ANN), Extreme Gradient Boosting (XGBoost), and logistic regression models used to identify significant predictors.
Results
A total of 413 high-level athletes were included (36 professional, 151 college, 226 high-school) and 5.1% of athletes underwent revision arthroscopic surgery. A combination of 3 variables optimized model performance: post-operative femoral head-neck offset, pre-operative HOS-SSS score, and post-operative alpha angle. The XGBoost model demonstrated the best accuracy (R2 = 97.4%) All models identified postoperative femoral head-neck offset as the most important variable in predicting the need for revision surgery, and the logistic regression model found it to the only statistically significant variable (Odds Ratio: 0.007, P = 0.027). A cutoff value of 6.35 mm was established for femoral head-neck offset. Athletes below this threshold underwent revision surgery at a rate of 15.1% compared to 4.1% of athletes above the threshold (P = 0.004).
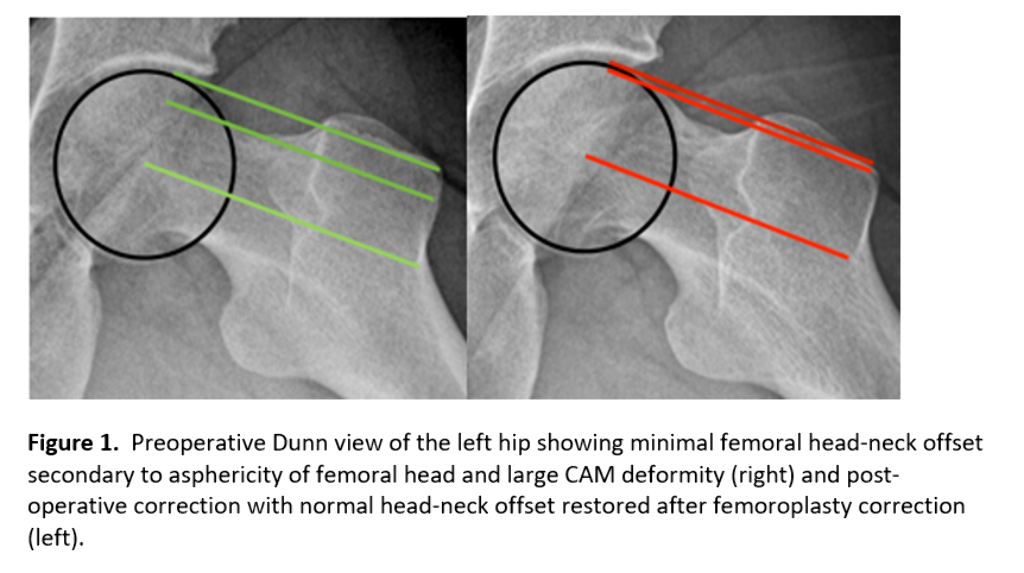
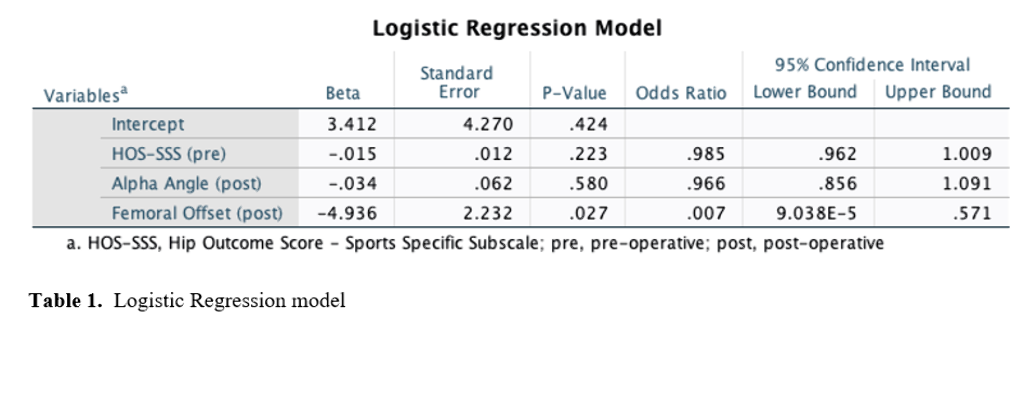
Conclusion
In a cohort of high-level athletes undergoing primary hip arthroscopy for FAIS, post-operative femoral offset was the most significant factor predicting revision hip arthroscopy with increased femoral offset resulting in a decreased likelihood of undergoing revision surgery.
Presenter Of 3 Presentations
P020 - Primary Segmental Labral Reconstruction for Irreparable Labral Tears in the Hip: Minimum Five-Year Outcomes
Abstract
Purpose
1) To evaluate minimum 5-year patient-reported outcome scores (PROs) in patients who underwent primary SLR with hamstring graft, in the setting of femoroacetabular impingement syndrome (FAIS) and irreparable labral tears, and 2) to compare the outcomes of hamstring autograft vs. allograft in a subanalysis using propensity-matched groups.
Methods and Materials
Prospectively collected data were retrospectively reviewed for patients who underwent primary hip arthroscopy from September 2010 to November 2015. Patients were included if they underwent SLR using hamstring autograft or allograft and had preoperative and minimum 5-year PROs. Exclusion criteria were previous ipsilateral hip surgery/conditions, dysplasia, or Tönnis grade > 1. Patients with autograft SLR were propensity-matched 1:1 based on age, gender, and body mass index (BMI) to patients who underwent SLR using hamstring allograft. The minimal clinically important difference (MCID), and patient acceptable symptomatic state (PASS) were calculated.
Results
48 hips were eligible to be included in this study, and 41 hips (85.4%) had minimum 5-year follow-up reporting significant improvement in all PROs. Fifteen of the 41 included patients underwent a SLR with a hamstring autograft and were matched to 15 patients with labral reconstruction using allograft hamstring. Groups were similar for gender (P >.999), age (P = .775), and BMI (P = .486). The average follow-up time was 80.8 ± 25.5 and 66.1 ± 8.3 months (P = .223) for the autograft and the allograft groups, respectively. Baseline PROs, preoperative radiographic measurements, surgical findings and intra-operative procedures were similar. The groups achieved significant and comparable improvement for all PROs (P < .0001), satisfaction (P = .187), and rate of achieving the MCID and PASS.
Conclusion
At minimum 5-year follow-up, patients who underwent primary arthroscopic SLR, in the context of FAIS and irreparable labra, reported significant improvement and comparable postoperative scores for PROs, patient satisfaction, MCID, and PASS using either autograft or allograft hamstrings.
P085 - Non-Arthritic Hip Pathology Patterns According to Gender, Femoroacetabular Impingement Morphology and Generalized Ligamentous Laxity
Abstract
Purpose
To identify hip pathology patterns according to gender, alpha angle deformity and generalized ligamentous laxity (GLL) in a non-arthritic patient population following primary hip arthroscopy for femoroacetabular impingement syndrome.
Methods and Materials
Patients who underwent primary hip arthroscopy between February 2008 and February 2017 were included and separated into males and females for initial analysis. The demographics, radiographic findings, intraoperative findings, and surgical procedures were then compared. A threshold of one standard deviation above the mean alpha angle in the male group was used to create two sub-groups. For females, GLL based on a Beighton’s score ≥4 was used to divide the group.
Results
A total of 2701 hips were included. Of those, 994 hips were in the male group and 1707 hips in the female group. Mean age was 36.6 years±13.8 and 37.1 years±15.0 for the male and female groups, respectively. The male group had a higher average alpha angle when compared to females [65.9°±11.9 vs 58.4°±10.8 (P<0.001)]. GLL was more common in females than males (P< 0.001). The male group had a higher proportion of acetabular Outerbridge grade 3 and 4 lesions compared to the female group (P<0.0001). Males in the alpha angle ≥78° sub-group reported higher rates of acetabular Outerbridge grade 4 damage than males in the <78° one (P<0.0001). Mean lateral center-edge angle was lower in the Beighton ≥4 female sub-group [23.7°±4.2 versus 31.3°±5.8 (P<0.0001)].
Conclusion
Two different patterns of hip pathologies were found to be related to gender. On average, male patients had higher alpha angles and increased acetabular chondral damage when compared to the females. A larger cam-type anatomy was associated with more severe acetabular chondral damage in males. In the female group, the incidence of features of hip instability such as GLL were significantly higher than in the male group.
P163 - Application of Deep Learning Models to Predict the Need for Revision Surgery in High-Level Athletes
Abstract
Purpose
To identify predictive factors for undergoing revision surgery in a cohort of high-level athletes undergoing primary hip arthroscopy for femoroacetabular impingement syndrome (FAIS).
Methods and Materials
Data were reviewed on all patients undergoing primary hip arthroscopy for femoroacetabular impingement syndrome (FAIS) between July 2008 and May 2019. Patients were included if they competed in professional, collegiate, and high school sports and had minimum 2-year follow-up for the Hip Outcome Score – Sport Specific Subscale (HOS-SSS). The primary outcome was undergoing arthroscopic revision surgery. Recursive feature selection was used to identify predictive variables from an initial pool of 27 features. A Multilayer Perceptron Artificial Neural Network (MLP-ANN), Extreme Gradient Boosting (XGBoost), and logistic regression models used to identify significant predictors.
Results
A total of 413 high-level athletes were included (36 professional, 151 college, 226 high-school) and 5.1% of athletes underwent revision arthroscopic surgery. A combination of 3 variables optimized model performance: post-operative femoral head-neck offset, pre-operative HOS-SSS score, and post-operative alpha angle. The XGBoost model demonstrated the best accuracy (R2 = 97.4%) All models identified postoperative femoral head-neck offset as the most important variable in predicting the need for revision surgery, and the logistic regression model found it to the only statistically significant variable (Odds Ratio: 0.007, P = 0.027). A cutoff value of 6.35 mm was established for femoral head-neck offset. Athletes below this threshold underwent revision surgery at a rate of 15.1% compared to 4.1% of athletes above the threshold (P = 0.004).
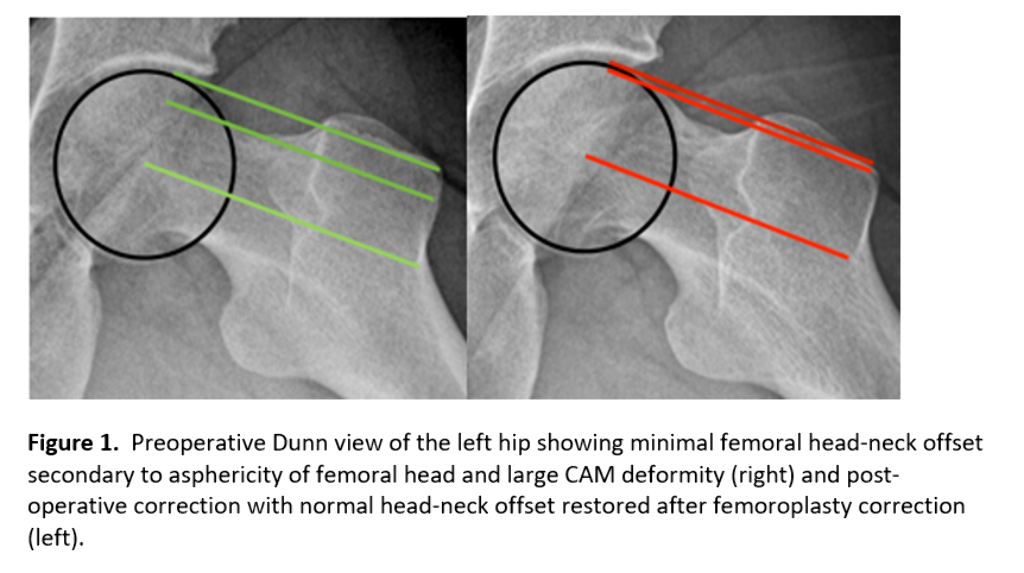
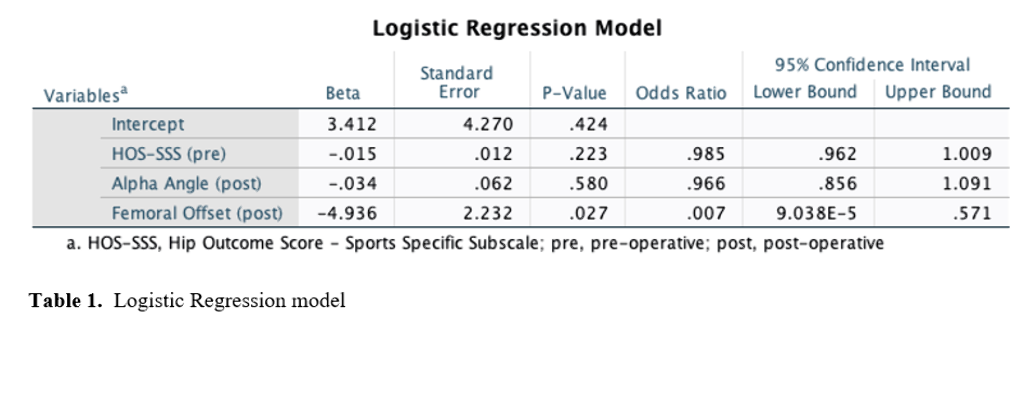
Conclusion
In a cohort of high-level athletes undergoing primary hip arthroscopy for FAIS, post-operative femoral offset was the most significant factor predicting revision hip arthroscopy with increased femoral offset resulting in a decreased likelihood of undergoing revision surgery.



