10.2.1 - Characterization of the Regenerative Effect of Lyophilized Hyperacute Serum in the Context of Osteoarthritis
Abstract
Purpose
Hyperacute serum is a blood-derived product that has demonstrated equivalent outcomes in osteoarthritis (OA) as the well-known platelet-rich plasma (PRP) in previous research. Moreover, hyperacute serum is a stable and standardized product, which overcomes the production disadvantages of PRP. In this study we focused on characterizing and defining a final lyophilized product and to test its regenerative capacities in tissue engineering in OA, alone and in combination with hyaluronic acid (HA).
Methods and Materials
Two-dimensional (2D) cultures of primary chondrocytes were kept in culture under different supplementation conditions, including three versions of hyperacute serum (one liquid and two lyophilized). XTT analysis and gene expression quantification were performed. Hyperacute serum was tested on a human co-culture of synovium, bone, and cartilage explants, previously inflamed. Cytokine profiles from supernatants were quantified and analyzed.
Results
Filtered lyophilized hyperactute serum did not present the same strong effect than the liquid format in promoting cell viability (P=0.0047). We hypothesize that due to the further filtration process, nutrients including growth factors were removed. Therefore, a new non-filtered lyophilized hyperacute serum was produced, which showed no significant difference in promoting cell viability when compared to the liquid format and PRP; furthermore, surpassing the supplementation gold standard FCS (P=0.03). Gene expression of OA-related genes including Col1a1, Col2a1, Acan, Sox9, Mmp3, Mmp13 and Prg4 presented high variability between patients, leading to not significant differences between the groups. However, a tendency suggesting that hyperacute serum supports more extracellular matrix protein secretion than PRP was noticed. Clusters of correlated cytokine and growth factor profiles were identified, showing that hyperacute serum controls inflammation significantly.
Conclusion
Non-filtered lyophilized hyperacute serum is a stable and standardized blood product with regenerative potential in the context of OA, maintaining the supplementation capacity of the liquid format and PRP.
10.2.2 - Directed Cell Migration by Superficial Zone Articular Chondrocytes in Response to Stable Growth Factor Gradients in a 3D Matrix
Abstract
Purpose
Purpose: Effectiveness of cartilage regenerative approaches are limited by the need to recruit and/or retain repair cells with the ability to form new cartilage tissue at the injury site. This study examines the chemotactic response of articular cartilage Superficial Zone cells to factors that might be used to bring chondroprogenitors to the transplant site, and/or to retain them on scaffolds or other delivery platforms.
Methods and Materials
Materials & Methods: A 3D hydrogel system was used to study chemotaxis by bovine Superficial Zone chondrocytes in response to stable gradients of an EGFR (Epidermal Growth Factor Receptor) ligand or an inflammatory chemokine, SDF-1α. Parameters of cell migration were quantified by time-lapse imaging in a novel chemotaxis assay system (iBidi) that recapitulates the unique requirements of slow-moving mesenchymal cells for stable, shallow chemotaxis gradients, and a 3-D matrix for adhesion-based movement.
Results
Results: Directed cell movement and overall efficiency of migration (Forward Migration Index) by articular cartilage Superficial Zone cells were optimal at the lowest concentration of EGFR ligand compared to SDF-1α. Chondroprogenitor velocity was increased in a dose dependent fashion with the highest concentrations of both factors revealing a chemokinetic (random movement) effect.
Conclusion
Conclusion: The kinetics of Superficial Zone chondrocyte chemotaxis through a physiologically relevant 3D matrix is consistent with the adhesion-dependent slow migration behavior characteristic of mesenchymal cells. Superficial Zone chondrocytes are extremely sensitive to chemotactic signals provided by EGFR ligand. We suggest this property could be leveraged to encourage recruitment or retention of chondroprogenitor cells at sites of cartilage injury/repair.
10.2.3 - Synovial Fluid MMP-1 and VEGF Concentration Correlates with Chondral Defects Severity and Symptoms in the Knee
Abstract
Purpose
This study sought to explore the correlations between preoperative synovial fluid biomarkers, cartilage structural characteristics on MRI, and pre- and postoperative PROs in patients undergoing chondroplasty for focal chondral defects.
Methods and Materials
This study prospectively enrolled patients undergoing chondroplasty for symptomatic focal chondral defects of the knee. Prior to the initiation of arthroscopy, synovial fluid was aspirated from the operative knee. Multiplex ELISA was then performed on the supernatant for several analytes. The relationships between biomarker concentrations, demographic factors, MRI findings as measured by AMADEUS score, and pre- and postoperative PROs were explored via independent t-test or Pearson correlation analysis. Variables significant on univariate analysis were included for multivariate linear regression.
Results
Cartilage defects of greater severity on MRI were significantly associated with increased concentration of MMP-1 and VEGF in synovial fluid (p<.05). Decreased preoperative KOOS Symptoms scores were correlated with increased concentrations of MMP-1 (r = -0.786, p<.001) and VEGF (r= -0.810, p<.001). These variables were non-significant on multivariate regression for KOOS Symptoms, although dominance analysis demonstrated that MMP-1 and VEGF were the greatest contributors to overall model fit, contributing 27.5% and 29.7%, respectively. Increased preoperative VEGF (r= -0.835, p=.019) and MMP-1 (r= -0.788, p=.036) were correlated with decreased improvement, or worsening of WOMAC stiffness score at 6 weeks after chondroplasty, while increased FGF2 (r=0.758, p=.049) and CCL2 (r= 0.777, p=.040) were positively correlated with improvement.
Conclusion
This study demonstrated that the concentration of MMP-1 and VEGF in synovial fluid correlate with cartilage lesion severity and may correlate with patient function and symptoms. These inflammatory biomarkers may be an important target in clinical practice towards improving outcomes when managing chondral defects of the knee.
10.2.6 - Histologic Grading Correlates With Inflammatory Biomarkers in Tibialis Posterior Tendon Dysfunction
Abstract
Purpose
The pathophysiology of pain in Tibialis posterior tendon dysfunction (TPTD) is not well understood. It has been theorized that TPTD is a degenerative process unrelated to inflammation. However, we hypothesize that inflammation is a key component of TPTD. The purpose of this study was to determine if inflammatory cytokines, matrix metalloproteases (MMPs), and glutamate were elevated in diseased TPTs.
Methods and Materials
Matched torn TPT, TPT insertion, and flexor digitorum longus (FDL) samples were collected from 21 patients with TPTD. The samples were individually incubated in media for 48 hours. The conditioned media was analyzed for inflammatory cytokines, MMPs, and glutamate. Histology was performed on the samples. Statistical analysis was performed with Friedman’s test and Wilcoxon-signed-rank post-hoc tests with Bonferroni correction (α = 0.0167). Spearman’s ρ was used to determine non-parametric correlations between histology and cytokine, MMP, and glutamate concentrations.
Results
Diseased TPT and TPT insertion groups were significantly elevated compared to healthy FDL for inflammatory cytokines IL-1β, IL-6, IL-8, IL-10, and TNF-α and MMPs MMP-1, MMP-2, and MMP-3 (p<0.005). Differences in glutamate concentrations were also significant, but only the diseased TPT group was significantly elevated compared to the healthy FDL tendons (p<0.01). Histologic grading correlated with inflammatory cytokine levels.

Conclusion
Diseased TPT and the TPT insertion demonstrated significantly elevated levels of inflammatory cytokines and MMPs compared to healthy FDL controls, suggesting a role for inflammation in the disease process. The amount of inflammation correlated with increased tendon degradation. The TPT, but not the insertion, contained significantly larger amounts of glutamate.
10.2.8 - Histological and Inflammatory Cytokine Analysis of OLT After Failed Microfracture, a Comparison to Fresh Allograft Controls
Abstract
Purpose
The purpose of this study is to characterize the structural and biochemical makeup of failed microfracture lesions in an effort to identify potential reasons for continued pain and poor OLT healing after microfracture as well as identify potential avenues for future research and early intervention.
Methods and Materials
Eight specimens were analyzed from symptomatic OLTs after microfracture who later underwent fresh osteochondral allograft transplantation. For each patient, the failed microfracture specimen and a portion of the fresh allograft replacement tissue were collected. The allograft served as a control. Histology of the failed microfracture and the allograft replacement were scored using the Osteoarthritis Research Society International (OARSI) system. Surface roughness was also compared. In addition, tissue culture supernatants were analyzed for sixteen secreted cytokines and matrix metalloproteinases (MMPs) responsible for inflammation, pain, cartilage damage, and chondrocyte death.
Results
The OARSI grade, stage, and total score as well as surface smoothness were significantly lower in the failed microfracture sample, indicating better cartilage and bone morphology for the allografts compared to the failed microfracture lesions. Analyzed cytokines and MMPs were significantly elevated in the microfracture tissue culture supernatants when compared to fresh osteochondral tissue supernatants.


Conclusion
The current study is the first to provide histologic and secretomic evidence demonstrating insufficiencies of osteochondral tissue after failed microfracture. These data demonstrate a significantly rougher cartilage surface, cartilage and subchondral bone histology that more closely resembles osteoarthritis, and elevated inflammatory cytokines and matrix metalloproteinases responsible for pain, inflammation, cartilage damage, and chondrocyte death when compared to fresh osteochondral allografts used as controls.
10.2.9 - Autologous Conditioned Plasma® Injections Provide Overall Limited Benefit for the Treatment of Knee Osteoarthritis
Abstract
Purpose
Autologous Conditioned Plasma (ACP®) (Arthrex®) is a commercially available platelet concentrate with positive results in available literature. We investigated the improvement after three injections with ACP® in a tertiary referral centre. Moreover, we studied the influence of the composition of the injections and of different patient factors as predictors of patient reported outcome measures.
Methods and Materials
We prospectively documented 261 patients (308 knees) receiving ACP® treatment for knee osteoarthritis (Figure 1). The improvement up to 12 months’ follow-up was measured using the Knee injury and Osteoarthritis Outcome Score (KOOS). ACP® composition was analysed for 100 patients. We evaluated the predictive value of age, sex, history (meniscus injury, anterior cruciate ligament rupture, cartilage defect, tibial plateau fracture), Kellgren and Lawrence grade, body mass index, and composition of ACP® using generalized estimating equations.

Results
KOOS improved from 36.7±13.6 at baseline (n=273) to 43.6±17.5 at 3 months (n=268), 43.6±17.8 at 6 months (n=238) and 42.0±17.7 at 12 months (n=216) (all p<0.01). An improvement above the minimal clinically important difference (MCID) was reached in 41% of patients after 6 months. Composition of the ACP® was variable (Figure 2), but did not correlate with KOOS. Among the evaluated factors, younger and more active patients presented lower improvements, while older age led to a higher clinical benefit (B=0.2, p=0.03). The lack of history of traumatic knee injury (B=3.8, p=0.04) also predicted better outcomes. No other factor significantly predicted outcomes in this series.
Conclusion
Treatment with ACP® leads to a significant improvement in KOOS, but this improvement is lower than previously reported in literature and does not reach the MCID in the majority of patients. Middle-aged patients with non-traumatic knee osteoarthritis may present better outcomes. The composition of ACP® varies between patients and within the evaluated range it does not predict outcomes. Patient selection might improve the potential of platelet concentrates.
10.2.10 - Leukocyte-Rich Versus Leukocyte-Poor Platelet-Rich Plasma for the Treatment of Knee Osteoarthritis: A Double-Blind Randomized Trial
Abstract
Purpose
Platelet-rich plasma (PRP) gained a large interest as a minimally invasive treatment for knee osteoarthritis (OA). Different preparation methods are available, and the presence of leukocytes, deemed detrimental from preclinical study results, is one of the most debated aspects regarding PRP efficacy. Aim of this study was to compare safety and effectiveness of Leukocyte-Rich PRP (LR-PRP) and Leukocyte-Poor PRP (LP-PRP) for the treatment of knee OA.
Methods and Materials
A total of 192 patients with symptomatic knee OA (Kellgren-Lawrence 1-3) was randomly allocated to 3 weekly injections of LR-PRP or LP-PRP. LP-PRP was obtained with a filter for leukodepletion. LR-PRP or LP-PRP were divided into aliquots of 5 mL with a mean platelet concentration of 1146.8x109/L and 1074.9x109/L and a mean leukocyte concentration of 7991.4x106/L and 0.1x106/L, respectively (Figure 1). Patients were evaluated at baseline and at 2-6-12 months with IKDC subjective score, KOOS subscales, EQ-VAS, and Tegner scores.

Results
Both LR-PRP and LP-PRP groups reported a significant clinical improvement at all evaluations performed up to 12 months. No differences were observed in terms of absolute values and improvement of the clinical scores at all follow-ups (IKDC subjective: 60.7±21.1 vs 62.9±19.9, respectively - Figure 2). No severe adverse events were described for both groups, while a total of 15 mild adverse events were reported: 4.7% for the LP-PRP and 12.2% for the LR-PRP group, without a statistically significant difference. No statistically significant difference was found between LP-PRP and LR-PRP in terms of failures (3.5%vs7.8%, respectively).

Conclusion
This double-blind RCT showed that three intra-articular LR-PRP or LP-PRP injections provided a significant and similar clinical improvement up to 12 months of follow-up in patients with symptomatic knee OA. Both treatment groups reported a low number of failures and adverse events, without inter-group differences. The presence of leukocytes did not significantly affect the clinical results of PRP injections.
10.2.11 - Anabolic Effect of LNA043: Results From an Imaging-Based Proof-of-Concept Trial in Patients with Focal Articular Cartilage Lesions
- B. Cole (Chicago, US)
- C. Scotti (Basel, CH)
- D. Laurent (Basel, CH)
- F. Saxer (Basel, CH)
- V. Juras (Vienna, AT)
- S. Trattnig (Wien, AT)
- S. Hacker (La Mesa, US)
- L. Pasa (Brno, CZ)
- R. Lehovec (Mladá Boleslav, CZ)
- P. Szomolanyi (Vienna, AT)
- E. Raithel (Erlangen, DE)
- J. Praestgaard (East Hanover, US)
- F. La Gamba (Basel, CH)
- J. L. Jiménez (Basel, CH)
- D. Ramos (Basel, CH)
- R. Roubenoff (Basel, CH)
- M. Schieker (Basel, CH)
Abstract
Purpose
LNA043 is a modified, recombinant human angiopoietin-like 3 (ANGPTL3) protein with chondro-anabolic effects on cartilage-resident cells and favourable safety profile. A first-in-human study demonstrated modulation of osteoarthritis-pathways, 7-Tesla magnetic resonance imaging (MRI) showed hyaline-like tissue-regenerates in a proof-of-mechanism study.
This study aimed at evaluating the chondro-regenerative capacity of intra-articular (i.a.) LNA043-injections in patients with cartilage lesions in the knee (NCT03275064).
Methods and Materials
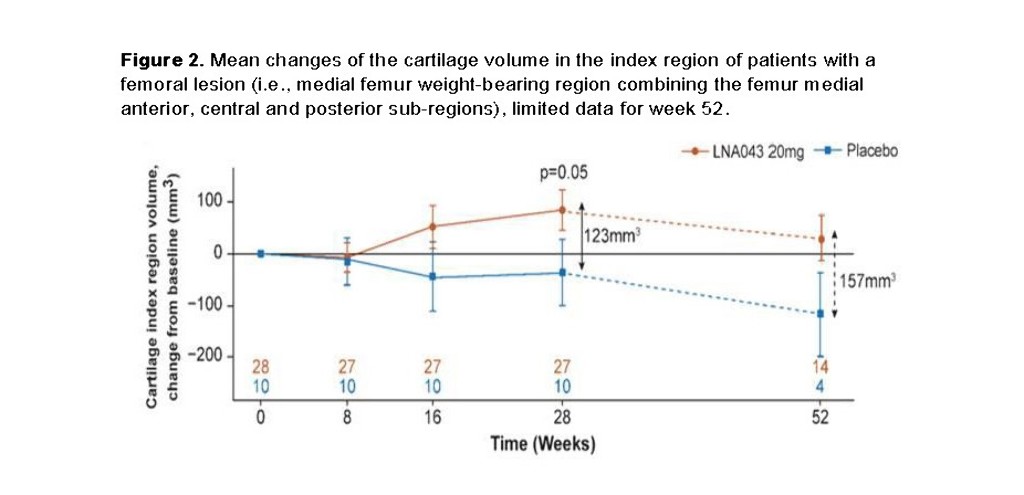
This randomised, double-blind, placebo-controlled, proof-of-concept study treated 58 patients with a partial thickness lesion (43 [20mg LNA043]; 15 [placebo]), stratified by condylar vs. patellar lesion with 4, weekly i.a. injections. T2-relaxation-time (primary endpoint) was assessed as marker of collagen-network organization, lesion-volume was a secondary endpoint, both using 3-Tesla MRI. Assessments were performed at baseline, weeks 8, 16, 28 and 52. Lesion-volume was determined from manual image-segmentation, the cartilage volume of 21 joint-spanning sub-regions was measured from 3D isotropic MRIs with automated segmentation (prototype MR Chondral Health 2.1 [MRCH], Siemens Healthcare, Figure 1). An exploratory analysis evaluated the volumetric treatment-effect on the 3 weight-bearing medial femoral sub-regions (index-region).
Results
No difference in T2-relaxation-time was detected at any timepoint. Manual segmentation showed continuous femoral lesion-filling in LNA043-treated patients up to week 28 (p=0.08, vs placebo) without effects on patellar lesions. MRCH demonstrated cartilage-volume increase in the index-region (∆=123mm3 at week 28, N= 37, p= 0.05, Figure 2) without overgrowth in the lesion-free lateral condyles. The safety profile was favourable; eight drug-related treatment emergent adverse events were reported after LNA043, one after placebo, mostly joint swelling (9.3% vs 0), resolving spontaneously or with paracetamol/NSAID. No anti-drug antibodies were detected.

Conclusion
Treatment with 4, weekly i.a. injections of 20mg LNA043 resulted in regeneration of damaged cartilage in patients with femoral lesions. Automated assessment of cartilage volume in the index-region was more sensitive than manual segmentation. A Phase 2b study in patients with knee OA is ongoing.



