Welcome to the ESPID 2022 Meeting Calendar
The Meeting will officially run on Eastern European Summer Time (Greece Time, CEST+1, GMT+2)
To convert the meeting times to your local time Click Here
Introduction
Artificial Intelligence in The Diagnosis and Management of Paediatric Tuberculosis
Artificial Intelligence in The Diagnosis of Pneumonia
Discussion
DESIGN AND IMPLEMENTATION OF A BREATH-RATE MEASUREMENT SOLUTION BASED ON COMPUTER VISION AND MACHINE LEARNING TECHNIQUES IN CHILDREN WITH LOWER RESPIRATORY INFECTION
Abstract
Backgrounds:
Camera-based diagnostic methods could allow an objective analysis of a patient's health remotely and contactless, which is especially interesting in telemedicine and pandemic scenarios. Artificial intelligence and computer vision can provide the diagnostic tools needed to improve patient monitoring. The main objective of this work is the design and implementation of a solution to estimate respiratory rate (RR) from a video captured through a smartphone, based on computer vision and deep learning techniques.
Methods
Prospective study of clinical information and a video of the patients’ chest with and without respiratory distress under 10 years old from November 2020 to May 2021 attending for a lower respiratory infection in a tertiary hospital in Spain. Video pre-processing was carried out using computer vision methods. As an initial approximation, remote photoplethysmographic signal (rPPG) was used with subsequent processing using the Discrete Wavelet Transform (DWT) and different methods to estimate the RR.
Results:
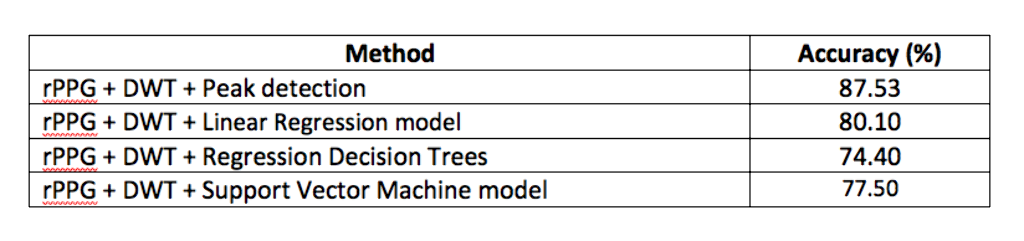
19 patients were included and 22 video sequences were pre-processed to carry out the estimation of the respiratory rate using the PPG signal approach. 51.3% were males and the average rate age was 2 years (DE 0.32). 61.5% patients had not relevant medical records. 48.7% were diagnosed of bronchiolitis followed by 30.1% diagnosed of asthma symptoms. Results obtained by different methods to estimate the RR can be seen in Table 1.
Conclusions/Learning Points:
It has been possible to design a breath-rate measurement solution to estimate RR from a video, based on DWT transformation to rPPG signal. This could be the first step in order to implement a breath-rate measurement solution based on computer vision and deep learning techniques.
PREDICTING SEVERE PNEUMONIA IN THE EMERGENCY DEPARTMENT: A GLOBAL STUDY OF THE PEDIATRIC EMERGENCY RESEARCH NETWORK (PERN)
Abstract
Backgrounds:
Pneumonia is a frequent and costly cause of emergency department (ED) visits and hospitalizations in children. No validated tools exist to assist with management decisions for children presenting to the ED with community-acquired pneumonia (CAP). Our objective was to develop prediction models to accurately risk stratify children with CAP across a global network of pediatric EDs.
Methods
Prospective study of children 3 months to <14 years old with CAP at 69 EDs in the Pediatric Emergency Research Network. We excluded children with recent hospitalizations, chronic conditions, or critically ill. The primary outcome was an ordinal composite of CAP severity occurring within 7 days: mild (discharged), moderate (hospitalized but not severe), and severe (empyema/effusion requiring drainage, ICU>48 hours, respiratory failure requiring positive-pressure ventilation, septic shock, vasoactive infusions, extracorporeal membrane oxygenation, or death). Multivariable logistic regression was used to develop risk models for moderate/severe disease (vs. mild) and for severe disease (vs. mild or moderate).
Results:
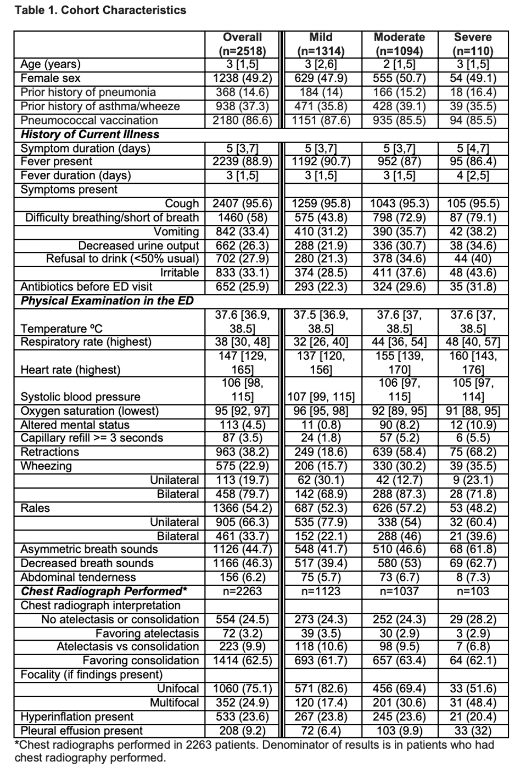
Of 2518 children, 1314 (52.2%) had mild CAP, 1094 (43.4%) moderate, and 110 (4.4%) severe (Table 1). Vomiting, elevated heart rate, elevated respiratory rate, oxygen saturation <90%, altered mental status, retractions, prolonged capillary refill, and pleural effusion were associated with development of moderate/severe CAP (Table 2). Elevated heart rate, asymmetric breath sounds, retractions, and pleural effusion were associated with severe CAP. The AUC for the moderate/severe model was 0.844 (95% CI, 0.828, 0.860) and for the severe model was 0.827 (95% CI, 0.792, 0.862).
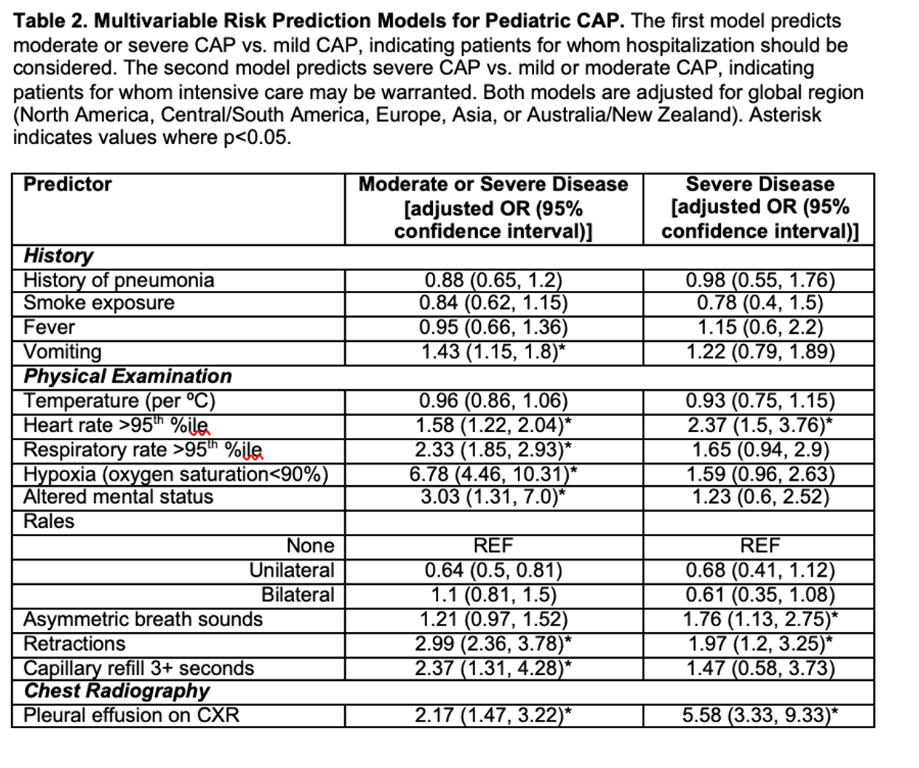
Conclusions/Learning Points:
We prospectively derived risk prediction models for pediatric CAP with features easily available at ED presentation in a global cohort of pediatric EDs. Both demonstrated excellent ability to predict moderate/severe disease warranting hospitalization, and severe disease for which intensive care should be considered.
