HYBRID CLOSED-LOOP SYSTEM IMPROVES GLUCOSE CONTROL IN PATIENTS TREATED WITH MULTIPLE DAILY INJECTION AND CGM OR INTEGRATED INSULIN PUMP AND CGM OR SENSOR-AUGMENTED PUMP
Abstract
Background and Aims
The MiniMed™ 670G Hybrid Closed-Loop (HCL) System improves glucose control and reduces glucose variability. There are no data whether HCL Systems achieve different results in T1DM patients treated with multiple daily injection and continuous glucose monitoring (MDI+CGM) or integrated insulin pump and CGM (CSII+CGM) or sensor-augmented pump therapy with predictive low glucose suspend (PLSG) feature. Aim of our study was to evaluate the effect on metabolic control of the switch from MDI+CGM, CSII+CGM or SAP with PLGS in type 1 diabetic patients.
Methods
Baseline clinical characteristics were presented as means and SD. One-way repeated measures ANOVA test was used to verify changes at 12 weeks from baseline in mean blood glucose, SD, TIR, TAR, TBR, Total Insulin dose and % of Basal Insulin.
Results
32 adults with type 1 diabetes (mean age 41,9 + 9,7; duration of diabetes 22 + 12,5; BMI 24,7 + 4,1), who had been using MDI + CGM (n=12) or CSII + CGM (n=11) or SAP therapy (n=9) were evaluated after switching to the 670G System. After 12 weeks a reduction of HbA1c (-0,39% p <0.001), mean glucose and SD (-9,7 mg/dl and 5,8 mg/dl p 0,003 and < 0,001) were observed. TIR increased significantly (+9,7% p < 0,001), in parallel with a reduction in TAR (-8,6% p 0,003) and TBR (-0,87% p 0,044).
Conclusions
Switching to the 670G System significantly improved glucose control in patients previously treated with MDI+CGM and CSII+CGM. Furthermore, similar results were obtained in patients treated with SAP with PLGS feature.
ADVANTAGES FROM “DO-IT-YOURSELF” LOOPS AMONG CHILDREN AND ADOLESCENTS AT VARNA’S DIABETES CENTER
Abstract
Background and Aims
In the last 5 years usage of automatic insulin delivery systems is increasing among patients with T1D. It has been shown that they improve metabolic control, decrease time spent in hypoglycemia and episodes of nocturnal hypoglycemia, increase time spent in target and are feasible and safe.
Aim: To evaluate benefits in children/adolescents using do it yourself (DIY) unapproved loops vs sensor-augmented pump therapy (SAP).
Methods
A total of 43 families with child/children with T1D on pump treatment and continuous use of CGM were invited to participate in the study;31 (72.1%) families accepted.The children were followed for 196 patient months.
Results
The study group consists of 31 children with T1D;24 of all are on SAP;7 use DIY loops. No differences were observed in both groups for age, duration of diabetes and daily insulin dose(Tabl.1) Patients on DIY loops spent significantly more time in range(83 vs 68.8%,p=0.02),less time in hyperglycemia above 14 mmol/l (2.1vs 8.6%,p=0.02) and have better HbA1c at 6th month(6.5 vs 7.2%,p=0.006 ) vs SAP patients for the follow-up period.No severe hypoglycemia and DKA occurred.There are no gender differences between and within both groups.
Tabl.1
| SAP | DIY loops | ||
| Age,y | 9.1±2 | 10.1±2 | NS |
| Duration T1D,y | 4.9±2 | 5.0±1.7 | NS |
| Insulin dose(U/kg/d) | |||
| initial | 0.83±0.2 | 0.76±0.2 | NS |
| present | 0.75±0.2 | 0.79±0.2 | NS |
Conclusions
DIY unregistered loops systems show promising results for better metabolic control without increasing the risk of severe hypoglycemia and DKA at least in terms of mean BGLs. Further impact e.g. consumed fat/protein, insulin dose,macro- and microvascular complications,etc.,remain to be studied in larger and longer studies.
AUTOMODE EXITS IN COMMERCIALIZED HYBRID CLOSED-LOOP SYSTEM
Abstract
Background and Aims
Hybrid closed-loop systems automatically deliver insulin based on sensor data. MiniMed 670G system operates in Auto Mode but exits to Manual Mode for certain reasons. The aim was to evaluate the duration, frequency and main reasons for exit from Auto Mode to Manual Mode.
Methods
Patients with type 1 diabetes using hybrid closed-loop system (Medtronic MiniMed 670G) for 3 months were evaluated. 2-week downloads were analysed to assess all the Auto Mode exits during this period of time.
Results
Data from 58 patients were included, age: 28 ± 15 years (7-63), 59% (n=34) females, diabetes duration: 15 ± 9 years, HbA1c: 7.0 ± 0.6%, TIR (70-180 mg/dl): 73 ± 9%.
Sensor use was 86 ± 13%. Time in Auto Mode was 85 ± 17%. Number of exits was 4 ± 2 per week (0.6 ± 0.3 per day). 16.8% of the exits were not explained. Sensor issues caused the majority of explained exits (39%), followed by hyperglycaemia (23%), auto mode disabled by user (16%) and maximum or minimum insulin delivery (13%). Frequency of exit reasons is shown in Figure 1.
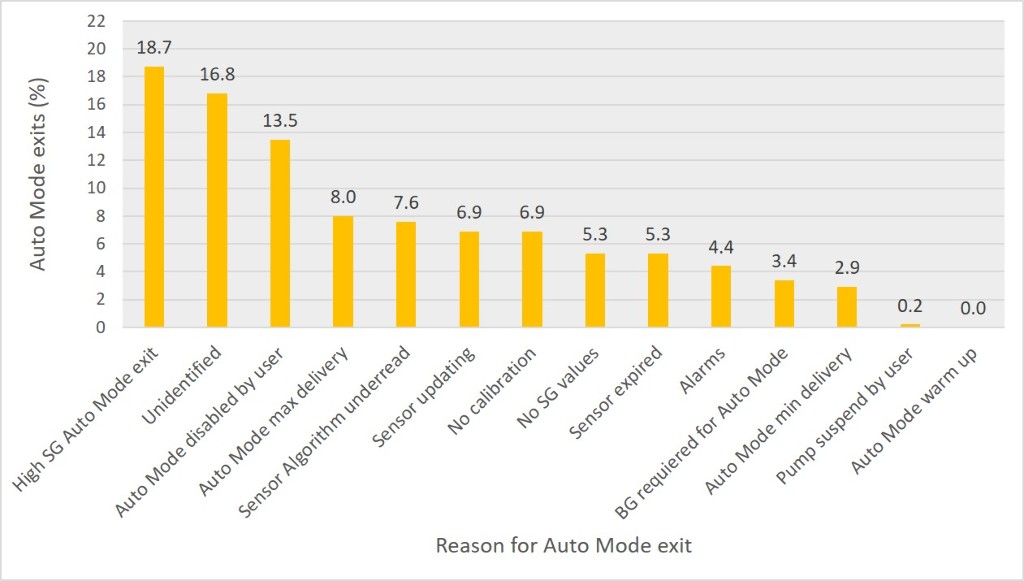
Conclusions
MiniMed 670G hybrid closed loop is maintained in Auto Mode during a high percentage of the time. The main reasons for exit to Manual Mode are sensor related, followed by high sensor glucose. A high percentage of exits are not explained. Time in Auto Mode should be maximized to improve the efficacy of the system and to avoid the burden of frequent interaction with the system for people with type 1 diabetes.
REAL-TIME BOLUS ASSISTANT FOR DIABETIC PATIENTS USING INSULIN
CREATE (COMMUNITY DERIVED AUTOMATED INSULIN DELIVERY): RANDOMISED TRIAL COMPARING AUTOMATED INSULIN DELIVERY (ANYDANA-LOOP) USING OPEN-SOURCE ALGORITHM, WITH SENSOR AUGMENTED PUMP THERAPY IN TYPE 1 DIABETES
Abstract
Background and Aims
Commercialised automated insulin delivery (AID) systems have demonstrated improved outcomes in type 1 diabetes (T1D), however they have limited capacity for algorithm individualisation, and can be prohibitively expensive if there is no access to health insurance or health funding subsidy. Freely available open-source algorithms with the ability to individualise algorithm parameters paired with commercial insulin pumps and continuous glucose monitoring make up the “do-it yourself” (DIY) approach to AID. Limited data on the DIY approach have shown promising results, but data from a large randomized control trial are lacking.
Methods
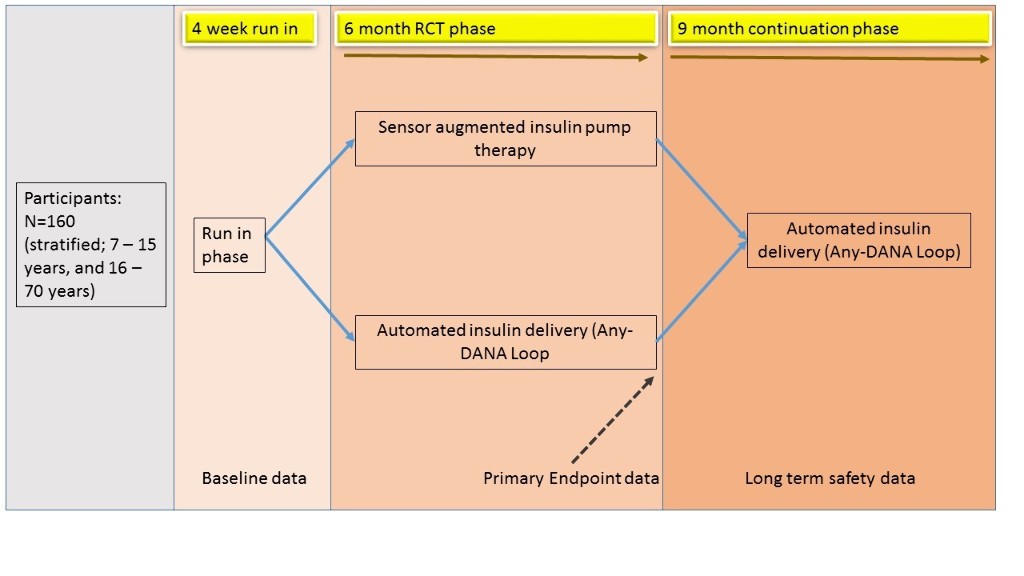
The CREATE trial is an open-labelled randomised parallel 6-month multi-site trial comparing the Android Artificial Pancreas System algorithm paired with the DANA-I insulin pump (SOOIL, South Korea) and Dexcom G6 (DexCom, San Diego) continuous glucose monitoring system (together named AnyDANA-Loop), compared to sensor augmented pump therapy. Participants (n=160) with T1D aged 7 – 70 years (age stratified into children/ adolescents 7 – 15 and adults 16 – 70 years), will be recruited from four sites in New Zealand.
Results
The primary outcome will be the time in sensor glucose range (3.9 -10mmol/L). A 9 month continuation phase follows to assess long-term safety (see figure). Secondary outcomes include psycho-social factors and platform performance. Analysis of online collective learning, characteristic of the DIY approach, is planned.
Conclusions
This study is funded by the Health Research Council New Zealand, with hardware support from SOOIL and DexCom. The CREATE trial will be prospectively registered and first participants are expected to be enrolled February 2020.
ADAPTIVE PERSONALIZED MULTIVARIABLE AP WITH PLASMA INSULIN CONCENTRATION ESTIMATION AND LEARNING OF UNANNOUNCED PHYSICAL ACTIVITIES AND MEALS
Abstract
Background and Aims
Most physical activities increase the risk of hypoglycemia for people with T1D. This study assesses the performance of our adaptive personalized multivariable artificial pancreas (AP-mAP) system without any exercises and meal unannouncements.
Methods
AP-mAP utilizes model predictive control, CGM readings, plasma insulin concentration (PIC) estimates and biosignals from a wristband. A patient’s historical data is leveraged to identify daily life activities using machine learning techniques. Incorporating online learning of probable times of significant glycemic disturbances from historical data improves AP performance by proactively mitigating the effects of impending disturbances. AP-mAP parameters such as controller set-point and PIC safety constraints are proactively modified for anticipated types and periods of disturbances.
Results
Simulations with the multivariable simulator mGIPsim illustrate the performance of AP-mAP. Twenty virtual subjects were simulated for 30 days with varying times and quantities of meals and different types, intensities, and durations of physical activities. AP-mAP reduced the 30-day average of total number of rescue carbohydrates from 20 to 6 without any hypoglycemia and improved glycemic control from 68.3% to 82.4% (in 70-180mg/dL range). One subject was simulated for 120 days with randomly varying times and quantities of meals and different types, intensities, and durations of physical activities (two exercise bouts per day). AP-mAP reduced the total number of rescue carbohydrates intakes for 120 days from 494 to 191 and kept good glycemic control (~83% in 70-180mg/dL range).
Conclusions
Integrating fully automated AP with machine leaning to adapt the AP and PIC during physical activities and meals improve diabetes management.
THE PERFORMANCE OF MINIMED 670G HYBRID-CLOSED LOOP DURING REAL-LIFE PROLONGED COMPETITIONAL TRAIL RACES (MOUNTAIN MARATHONS AND HALF-MARATHONS)
Abstract
Background and Aims
There are limited reports of the performance of the Minimed 670G hybrid-closed loop (HCL) during prolonged continuous effort. The aim of this report was to assess the performance of the HCL in maintaining time-in-range and avoiding hypoglycemia during mountain trail running races.
Methods
A type 1 diabetic recreational athlete wearing the HCL system participated in two marathons and one half-marathon. Time-in-range (TIR), average sensor glucose (ASG) and hypoglycaemia were analysed during the entire races, first 2h and remaining hours (only marathons). Carb supplementation was used to prevent/treat lows and replenish energy stores.
Results
No hypoglycemia was recorded. Time-in-range for the marathons (10h47’ and 6h15’) and half-marathon (2h23’) was 83%, 79% and 19%, with ASG of 143.3 mg/dl, 143.8 mg/dl and 232 mg/dl, respectively. During the first 2h of the marathons, TIR and ASG were 68% with 153.96 mg/dl and 52% with 184.36 mg/dl, respectively. During the rest of the races, TIR and ASG were 87% with 140.64 mg/dl and 92% with 123.67 mg/dl, respectively.
Conclusions
The 670G HCL avoided hypoglycemia during all races. Longer races correlate with an increase of TIR and decrease of ASG. Race difficulty (positive level difference, speed, route) impacts the loop’s ability to maintain glycemia in range. High intensity intervals overshoot glucose levels and cannot be rapidly countered by the algorithm. Certain strategies (insulin bolus at the start of race) are required to prevent hyperglycemia resulting from the adrenalin rush at race start. The HCL dramatically reduces hyoglycemia risk during prolonged continuous physical activity while increasing TIR.
HYBRID CLOSED LOOP IMPROVES GLYCAEMIC CONTROL IN GASTROPARESIS IN TYPE 1 DIABETES
Abstract
Background and Aims
Growing numbers of UK patients have been using the Minimed 670G Hybrid Closed Loop system since European commercialisation in 2018, with clinical "real world" experience extending beyond the initial data available from initial pivotal studies. Gastroparesis is a challenging complication which makes control of glycaemia difficult even with sensor augmented pump therapy. We report here our initial clinical experience with using the 670 in a subset of people with type 1 diabetes with advanced complications including gastroparesis.
Methods
We analysed data from 6 patients (all females already using insulin pumps, aged 47 + 4, diabetes duration 27 + 3 years, laboratory HbA1c 78 + 3 mmol/mol) started on 670G system as part of our clinical service from December 2018 onwards. All had both gastroparesis and multiple other complications of diabetes including laser-treated retinopathy, nephropathy, foot ulceration, faecal incontinence secondary to autonomic neuropathy, cerebrovascular accidents and angina. Gastroparesis had remained problematic in all despite optimised care (including intragastric botox injections and pyloroplasty in one individual and insertion of a gastric pacemaker in another). We compared data from sensor augmented pump therapy immediately prior to activating automode (closed loop) with subsequent data captured during automode.
Results
Time in range (3.9 to 10 mM) increased markedly from 35 + 3 % (consistent with challenging gastroparesis) to 64 + 4% at most recent downloads (average time using 670 system 7 + 1 month).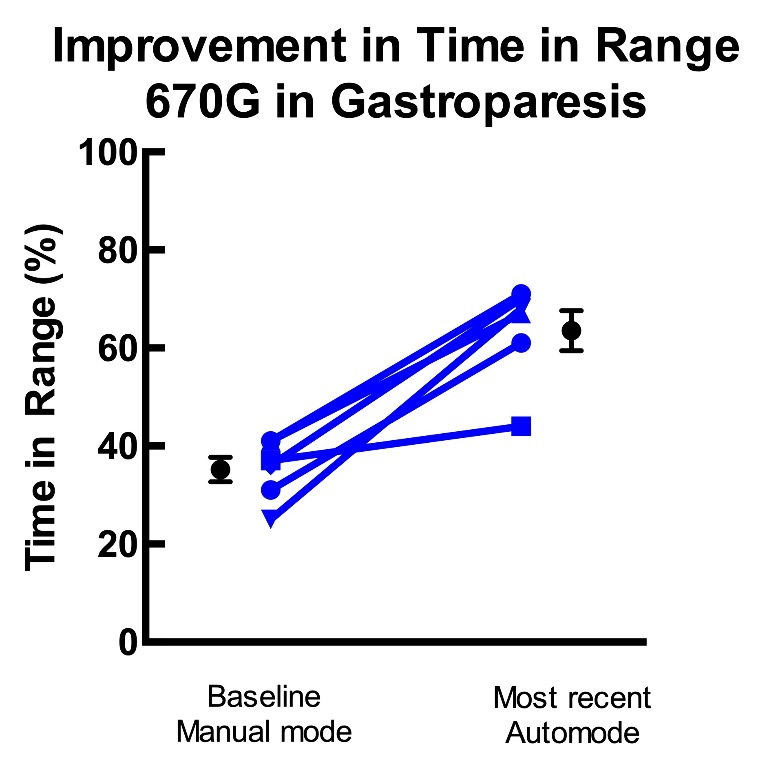
Conclusions
Hybrid closed loop insulin delivery may be extremely effective in improving glycaemic control even in those with gastroparesis and erratic glucose control.
PEDIATRIC GLUCOSE REGULATION WITHOUT PRE-MEAL INSULIN BOLUSES: AN APPROACH BASED ON SWITCHED CONTROL AND TIME-VARYING IOB CONSTRAINTS
Abstract
Background and Aims
AP systems have shown to improve glucose regulation in T1D patients. However, full closed-loop performance remains a challenge particularly in children and adolescents, since these age groups often present the worst glycemic control.
Methods
In this work, a new algorithm based on switched control and time-varying IOB constraints is presented (ARGAE). This method is a combination of ideas from the previously introduced Automatic Regulation of Glucose (ARG) algorithm, which features no pre-meal insulin boluses [1], and the Amplitude Enable (AE) mode, which allows the controller to act more aggressively at the beginning of meal intake without risking postprandial hypoglycemia [2]. The proposed control strategy is evaluated in silico and its performance contrasted with the ARG algorithm in the pediatric population.
Results
The in silico tests performed indicate that the use of the Amplitude Enable layer can help increase the time in euglycemia for both adolescent and children age groups (see tables 1 and 2). Hypoglycemia is significantly reduced in children and completely avoided in adolescents. This is an important upside of the ARGAE since a severe hypoglycemia episode is one of the most dangerous situations for people with T1D.
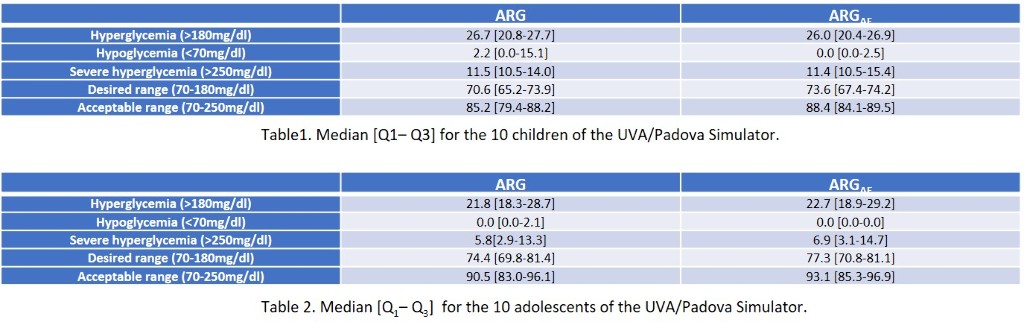
Conclusions
Simulations show that the proposed algorithm improves the performance of the ARG algorithm.
[1] P. Colmegna, F. Garelli, H. D. Battista and R. Sánchez-Peña, Control Engineering Practice, no. 74, pp. 22-32, 2018.
[2] E. Fushimi, N. Rosales, H. De Battista and F. Garelli, Biomed Signal Process Control, vol. 45, pp. 1-9, 2018.
ONLINE ADAPTATION OF FUNCTIONAL INSULIN THERAPY PARAMETERS IN SUBJECTS WITH TYPE 1 DIABETES MELLITUS: IN-SILICO RESULTS OF A DATA-DRIVEN METHOD
Abstract
Background and Aims
Functional insulin therapy (FIT), i.e., adjusting meal insulin to estimated meal carbohydrate (CHOmeal) and pre-meal blood glucose (BGmeal), is the recommended approach for prandial insulin dosing. However, the choice of FIT parameters (i.e., insulin-to-carbohydrate ratio [CR] and correction factor [CF]) remains challenging. Here, we propose a novel data-driven method for the online adaptation of FIT parameters.
Methods
A multi-step method was developed. A linear model of postprandial minimum glycemia (PMBG) is built, with BGmeal, CHOmeal, CR and CF as model predictors. At every meal, the model is identified using recursive least squares; simultaneously, distributions of CHOmeal, BGmeal and model error (all assumed normal) are updated. At every weekly adaptation run, optimal CR and CF are derived by minimizing the variance of PMBG, imposing 5% of PMBG values <70mg/dl. To test the method, a 10-week in-silico study was built using the UVA/Padova simulator. One-hundred virtual adults received 3 meals/day of random size, with 50% carbohydrate counting error, and meal boluses delayed up to 60min. Hypoglycemia treatments were administered at glycemia <70mg/dl. The method (initialized with random error on CR and CF) was compared to the subjects’ original FIT parameters.
Results
The evolution of glycemic outcomes is shown in the figure. At week 10, average time in 70-180mg/dl, <70mg/dl, and >180mg/dl, and number of hypoglycemia treatments/day were (original–adapted parameters): 82.6%–83.7%, 2.8%–0.4%, 14.7%–16%, and 2.3–0.3.
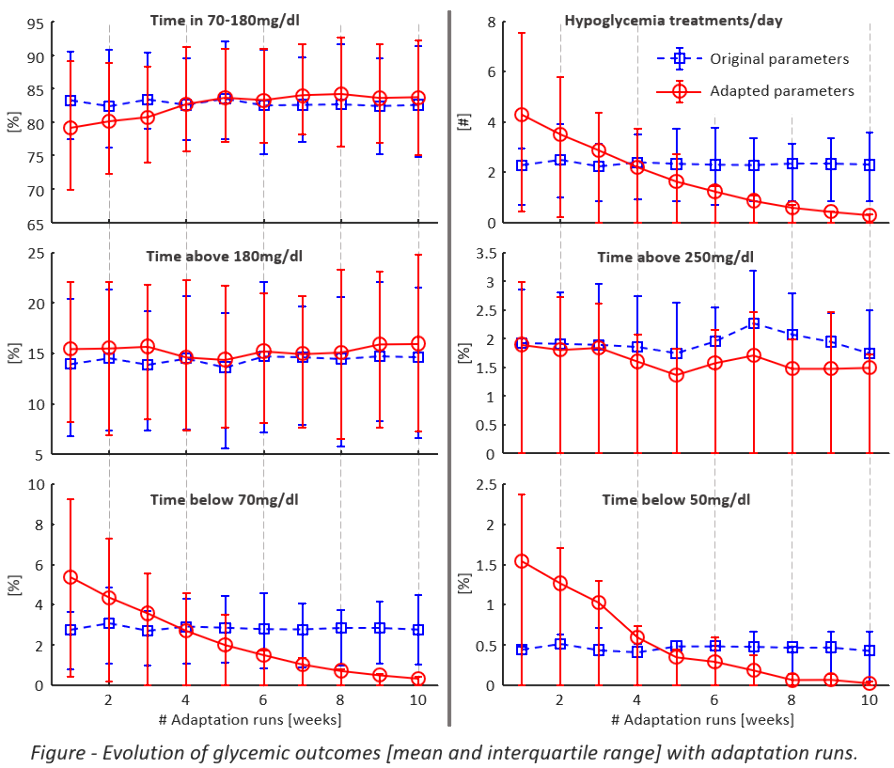
Conclusions
The novel approach to optimize FIT parameters corrects for suboptimal CR/CF and improves glycemic outcomes in a simulation environment; further studies are needed to assess its robustness for real-life applications.
FIRST ITALY DIY APS USERS SURVEY
Abstract
Background and Aims
Do-it-Yourself Artificial Pancreas Systems (DIYAPS) are becoming popular among people with diabetes of all ages and countries. We don’t have any information regarding italian situation. Aim of the study was to obtain a first photograph of the Italian loopers community.
Methods
An online survey (18 items) was distributed (July 2019) to DIY users/planning recruited through the Facebook groups Looped and OpenAPS.
Results
139 adults responded to the survey: 120 were interested in and 19 users (5 under the age of 18). The users (5 in open, 12 in closed loop) were 45% female and the mean age was 28.1±16.9, range 2-60yrs; duration of diabetes 14.7±10.6yrs. 58% of pts had been using DIYAPS for less than 6 months; 26% for over 1 year. AndroidAPS and Loop were more used than OpenAPS (8, 9 and 2 pts, respectively). Omnipod was the most used pump (50% of pts); AccuChek, Medtronic, Tandem and Dana pumps were used respectively by 25, 15, 5 and 5% of pts. 80% of pts (100% of pediatrics) used CGM Dexcom systems. The most frequent reasons for using/planning the DIY were: to improve my control, to sleep better, to have a more discreet system, usable by phone/smartwatch, to reduce hypoglycemia. Finally, the 60% of responses said that they had received a positive or neutral response from their clinic.
Conclusions
This first survey demonstrates the use of DIY systems is also spreading in Italy and that the interest of patients is rapidly increasing.
PROFILED GLUCOSE FORECASTING USING GENETIC PROGRAMMING AND CLUSTERING
Abstract
Background and Aims
This research is motivated by the challenge of creating a general method to accurately predicting future glucose levels, so, an automated or manual system can decide when and how much insulin to inject in order to maintain glucose levels within a healthy range. It is imperative to avoid predictions that may trigger unnecessary treatments or, even worse, treatments that are harmful to the patient.
Methods
The proposed methodology is a three-step process: Data collection, preprocessing, and division, Data clustering and detection of a set of glucose profiles, and, Models training, creating models by evolutionary computation. CHAID (CHi-square Automatic Interaction Detection) is applied to recursively divide the data in relation to a target variable using multiple divisions between the different input variables: days of the week and time slots. A data augmentation algorithm hat generates synthetic glucose time series is used in training datasets to develop meaningful information and significantly enhance data quality. Next, models based on Genetic Programming (GP) are created using cross-validation. Then, the best model of 10 repetitions is selected by the Akaike Information Criterion (AIC).

Results
Data was collected from ten patients. The predictors used in the construction of the tree are the day of the week and the time slot. Significant differences were observed in the glucose profiles classified for each of those categories.
Conclusions
The accuracy of predictions with models created with GP is better for shorter time horizons and gradually gets worse as the time horizon increases from 30 to 240 minutes.
Thanks: RTI2018-095180-B-I00 and Fundación Eugenio Rodriguez Pascual
GLUCOSE FORECASTING WITH RANDOM GRAMMATICAL EVOLUTION
Abstract
Background and Aims
Bolus decision is a difficult task since patients need to estimate the number of carbohydrates they are going to ingest, take into account the past and future circumstances, know the past values of glucose, evaluate if the effect of previously injected insulin has already finished and any other relevant information. In this work, we present and compare a set of methodologies to automate the decision of the insulin bolus, which reduces the number of dangerous predictions.
Methods
We combine two different data enrichment techniques based on Markov chains with grammatical evolution engines to generate models of blood glucose, and univariate marginal distribution algorithms and bagging techniques to select the set of models to assemble. Modeling is solved as four symbolic regression problems by Random-Grammatical Evolution.
Results
We report the Clarke’s Error Grid Analysis.The best results are obtained with an ensemble model developed by bagging of 100 models. For a 30 minutes forecasting horizon, all the strategies have similar performance with almost no points in the D and E zones. For the 60, 90 and 120 minutes, the best models are produced by Random-GE and Bagging with both data augmentation techniques, obtaining a 95% of safe predictions,on average.
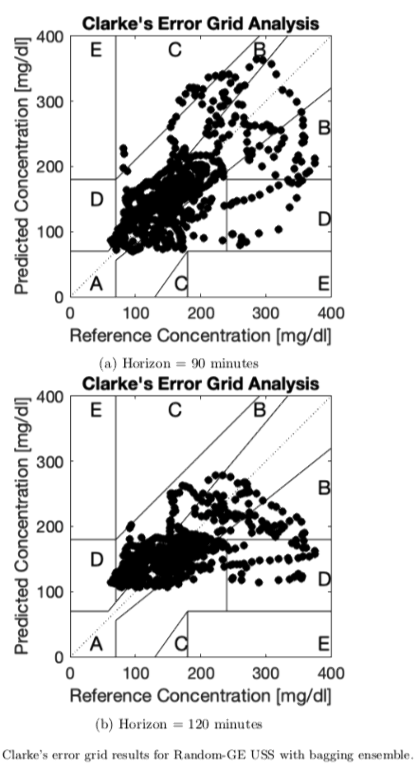
Conclusions
Results show how the methods improve results from pre-vious works. The proposal uses a simplified preprocessing process of the raw data, we use symbolic regression standard grammars and execution times are low. In future works, we should move a step forward in the forecasting horizon.
Thanks: RTI2018-095180-B-I00 and Fundación Eugenio Rodriguez Pascual
EFFECTS OF WHEAT BRAN DIET AND MAIZE BRAN DIET ON THE RANDOM BLOOD GLUCOSE AND WEIGHT OF ALLOXAN INDUCED DIABETIC RATS
Abstract
Background and Aims
The present study was conducted to evaluate the effect of wheat and maize brans feeds on the random blood glucose of the rats. These feeds were prepared using the the Purified Diet AIN-93-G with some modifications.
Methods
The experiment was laid out under completely randomized design. The rats (n=24) of almost uniform age and weight were divided into 4 groups each containing 6 rats. Group I comprised rats with normal blood glucose level reared on basal diet (AIN-93-G), Group II was Alloxan monohydrate (ALX monohydrate) induced diabetic rats reared on Purified Diet AIN-93G. Group III comprised Alloxan monohydrate induced diabetic rats fed a wheat bran diet and Group IV consisted of Alloxan monohydrate induced diabetic rats reared on a maize bran diet. The Random Blood Glucose (mg/dL) of these groups was monitored at the end of each week for a period of 6 weeks.
Results
Bran diets (maize and wheat) significantly lowered the Random Blood Glucose level in the experimental animals. However,the group of rats fed on maize bran diet had a significantly (p<0.05) more pronounced glucose lowering as compared to the group of rats fed on wheat bran diet.
Conclusions
The results indicated that both wheat and maize bran exert anti-diabetic effects on the ALX monohydrate induced diabetes and therefore, can be a part of diet based therapy for the management of diabetes.
REINFORCEMENT LEARNING BASED INSULIN BOLUS CALCULATOR: IN SILICO STUDY
Abstract
Background and Aims
Despite the development of artificial pancreas, many diabetics are using insulin injection devices. And about 80% of insulin delivery products are bolus injection devices and the rate of used as home care is higher than the rate used in hospitals and clinics. Therefore, insulin bolus calculation algorithm for insulin injection devices will be helpful for many diabetics. In this study, we propose a reinforcement learning based bolus calculation algorithm.
Methods
We determine the injection timing of insulin bolus through the PK/PD (pharmacokinetics/pharmacodynamics) curve of OGTT (Oral Glucose Tolerance Test) and the GCT (Glucose Clamp Test). And injection amount of insulin bolus is determined before each three meals using DQN (Deep Q-Networks) reinforcement learning algorithm. Basal insulin is injected with an optimal amount. Also, to learn the method to prevent hypoglycemia more effectively, snacks are not allowed before bedtime and higher penalty is given in hypoglycemia. The proposed method is evaluated on one adult from the US-FDA approved UVa/Padova simulator under a multi-meal scenario.
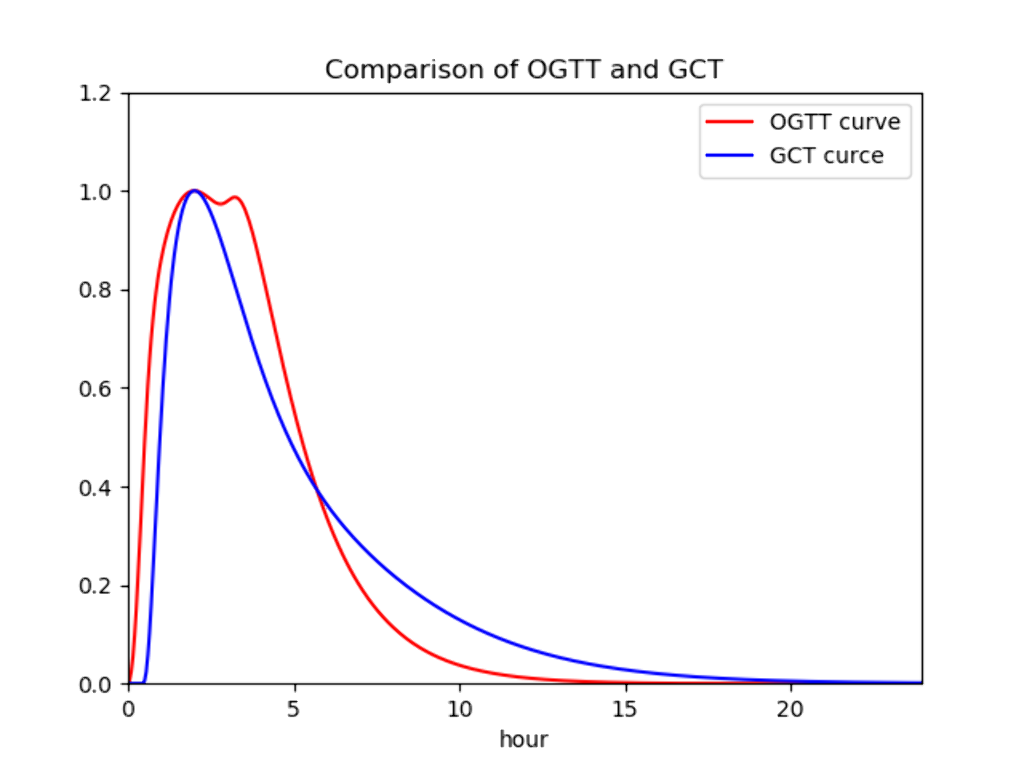
Results
The insulin bolus calculation algorithm achieves a mean glucose of 114.54 mg/dl and a time in range of 89.30%. Insulin is injected 25 minutes before each meal and the algorithm showed a tendency to change the amount of insulin injection according to the amount of meal.
Conclusions
The reinforcement learning based insulin bolus calculation algorithm is effective in determining the amount of insulin bolus according to the amount of food and the personalized insulin injection timing according to PK/PD characteristics.
MODEL CONFORMANCE IN BLOOD GLUCOSE PREDICTION TASKS
Abstract
Background and Aims
In recent years, neural network models (NNMs) have gained popularity for use in predicting blood glucose (BG) values. These models have the advantage of being data-driven and trained to model an individual's unique physiological characteristics. However, NNMs remain opaque and difficult to understand and interpret by human users. In this work, we address a key challenge in designing and training NNMs for BG prediction: ensuring NNMs conform to known physiological dynamics. We demonstrate how the standard learning protocol results in non-conformant models, and present a physiologically-motivated learning approach to ensure conformance is obtained without sacrificing accuracy.
Methods
Using a combination of mixed integer programming and local gradient search, maximum and minimum changes in predicted BG corresponding to increased insulin infusions are tested in three classes of NNMs: a generalized NNM structure, and two novel physiologically motivated structures. Model sensitivity of each input is computed and tested for conformance to "increased insulin results in decreased BG values". Models are trained using previously collected CGM and insulin pump data from a cohort of twenty-four subjects with T1D to predict 60min horizons.
Results
Accuracy, computed by root mean square error, remains consistent across all models [Table 1]. However, only the constrained, physiologically motivated model fully conforms to "increased insulin decreases BG" [Fig. 1].
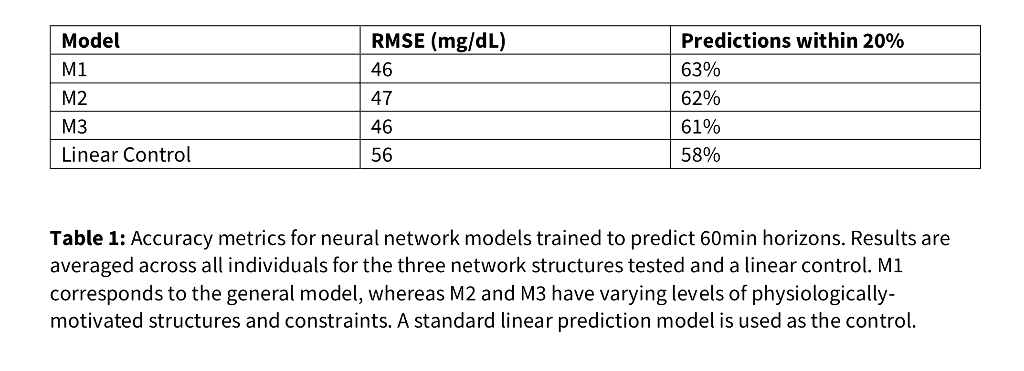
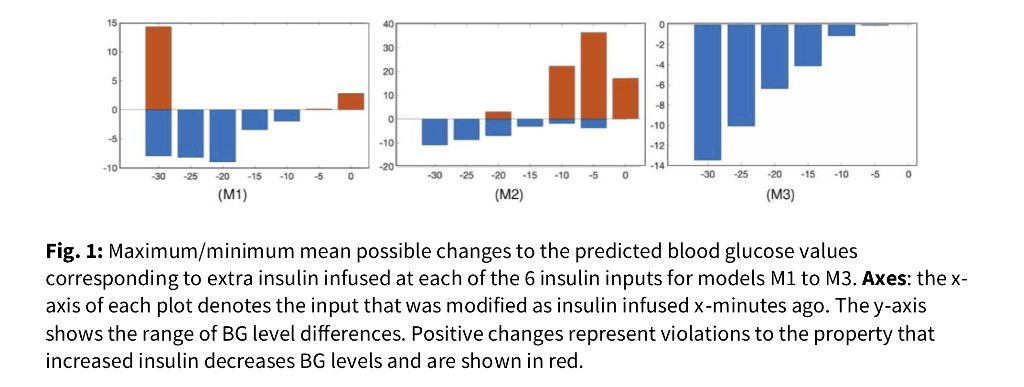
Conclusions
A novel test for conformance of NNMs to known physiology is presented. We demonstrate how standard NNMs learned for BG prediction can fail to conform, and present a physiologically motivated design to learning which improves conformance while maintaining accuracy.
TRANSLATING STANDARD CLINICAL PROTOCOL INTO TUNING PROCEDURES FOR HYBRID CLOSED LOOP SYSTEMS: 670G, CONTROL-IQ AND LOOP
Abstract
Background and Aims
The transition of new hybrid closed loop (HCL) artificial pancreas systems from research into widespread clinical use brings exciting advances to diabetes care. However, tuning protocols for current and in-trial systems vary significantly. This work seeks to establish a comprehensive guide for clinicians for translating clinical practice into tuning procedures for patients on the Medtronic 670G, Tandem Control-IQ, and Do-It Yourself (DIY) Loop systems.
Methods
Retroactive patient data, in-silico HCL implementation, algorithmic analysis and clinical experience is utilized to correlate features in blood glucose profiles with adjustments in HCL parameters leading to improved control. Parameters and tuning protocols for the Medtronic 670G, Control-IQ, and DIY Loop systems are compared against standard clinical guidelines for setting basal rates, insulin sensitivity, correction factors, carb ratio, and additional control set points when applicable.
Results
Tuning procedures for each parameter setting across devices, with detailed descriptions and simplified tables will be presented. Figures demonstrating effects of parameter changes on insulin dosing for each system, along with cases for when to adjust a certain parameter will be shown. In all we find 2 adjustable parameters in 670G, 5 in Control IQ and 10 in Loop. Fig. 1 depicts an example table for one parameter: "Target Range".
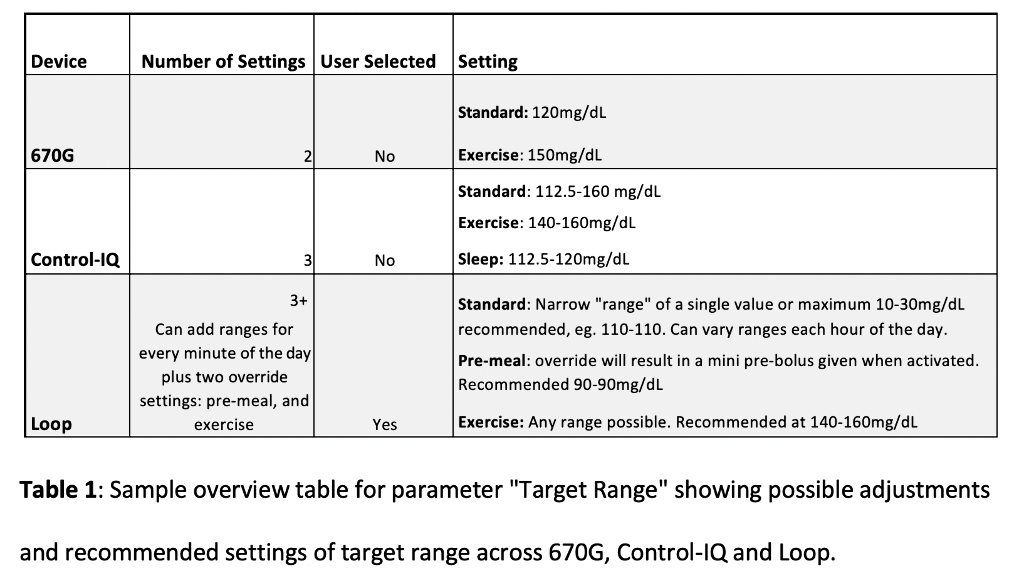
Conclusions
As additional HCL systems enter the clinical market and popularity of DIY systems grows, it is vital for clinicians to understand differences and similarities between systems. This work helps translate standard clinical adjustments into sequences of parameter tuning for each HCL system in order to provide a comprehensive guide for clinicians.
COMPARING DIY FULL CLOSED-LOOP PERFORMANCE IN PIGS WITH STREPTOZOCIN-INDUCED DIABETES
Abstract
Background and Aims
Do-It-Yourself (DIY) algorithms for closed-loop insulin delivery are increasingly popular but infrequently studied in humans, outside of observational studies, due to lack of regulatory approval. We therefore conducted studies in pigs comparing AndroidAPS and Loop without meal announcement, leveraging faster insulin pharmacokinetics inherent to swine.
Methods
Pigs with streptozocin-induced diabetes were started on AndroidAPS running oref1 (with super-microbolus enabled) and Loop (with integral retrospective correction enabled). Insulin dosing including basal rate, insulin-to-carbohydrate ratio (ICR) and insulin sensitivity factor (ISF) were determined clinically prior to closed-loop initiation. Insulin pharmacokinetics were derived by ELISA and observation of glucose dynamics. Basal rate testing was conducted overnight without insulin-on-board (IOB) or carbs-on-board (COB) and rates were titrated to maintain glucose. ISF was calculated by administering 1 unit insulin under hyperglycemic conditions with no IOB or COB. ICR was calculated and then titrated such that post-meal blood sugar matched pre-meal.
Results
6 pigs were started on AndroidAPS followed by Loop. Insulin pharmacokinetics are more rapid in pigs with peak serum concentrations within 20-25 minutes and near complete absorption by 2 hours, modeled in both systems. In total, there were 23 days of AndroidAPS and 18 days of Loop data. Time-in-Range (70-180mg/dL) was significantly greater (p < 0.001) with AndroidAPS (63.7 ± 13.4%) versus Loop (40.5 ± 17.2%).
Conclusions
For unannounced meals, Time-in-Range was greater with AndroidAPS than with Loop. oref1 with super-microbolus is designed for unannounced meals, whereas Loop is a model predictive controller with short-term adaptation more dependent on meal data.
REINFORCEMENT LEARNING BASED AUTOMATED INSULIN INFUSION: IN SILICO FEASIBILITY STUDY
Abstract
Background and Aims
For an advanced artificial pancreas, the automation of insulin treatment is of great interest in clinical and research aspects. Despite recent algorithmic advances, there are fundamental challenges to overcome, such as uncertainties from unannounced meals and delays from "insulin stacking." In this study, we propose a reinforcement based automated insulin infusion algorithm.
Methods
We devise a bio-inspired reinforcement learning approach where a reward function mimics the temporal homeostatic objective of β-cells and a discount rate reflects individual specific pharmacokinetics/pharmacodynamics (PK/PD) characteristics. The proposed method is evaluated on 10 adults from the US-FDA approved UVa/Padova simulator under a single-meal with preprandial fasting scenario.
Results
The trained algorithm achieves a mean glucose of 117.21 mg/dl. At the beginning of the fasting phase, the average patient's sensor glucose is 121.61 mg/dl, and it is stabilized to basal state with 100.41 mg/dl under the automated regulation. For the postprandial phase without any meal announcement, the trained algorithm automatically regulates the postprandial glucose with a sudden peak of the insulin infusion rate which is followed by a gradually decreasing rate. About three hours after meal-intakes, the infusion rate becomes the lowest and results the patients to avoid hypoglycemia.
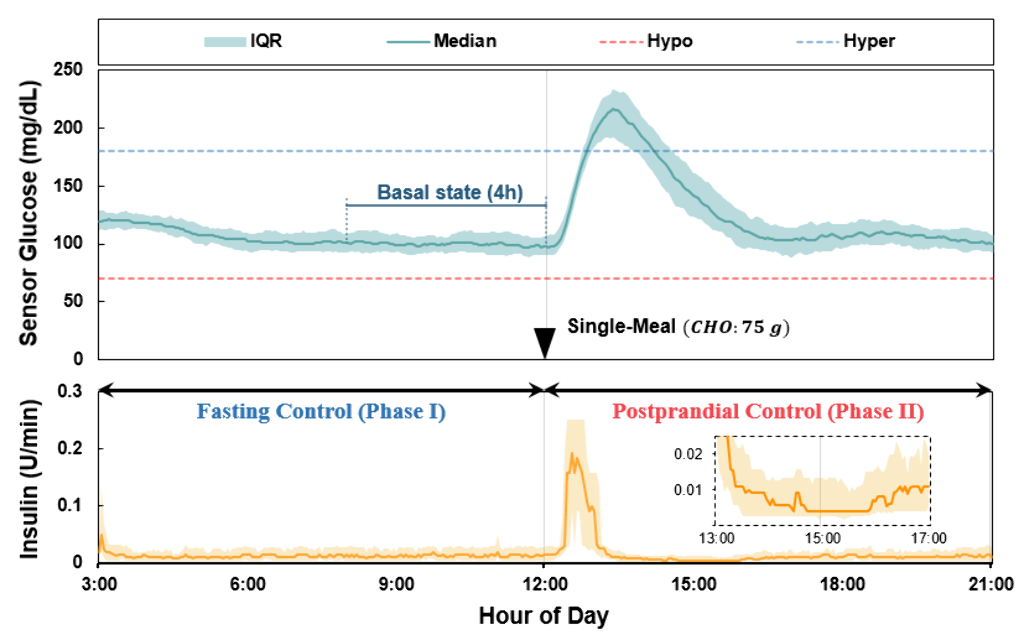
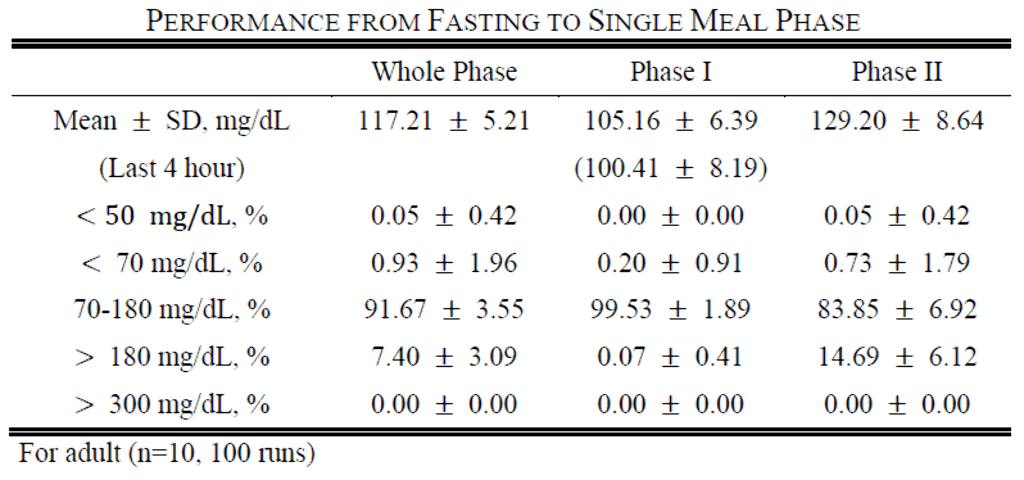
Conclusions
The proposed insulin infusion algorithm based on the bio-inspired reinforcement learning approach allows for fully automated glucose control with hypoglycemic avoidance.
Acknowledgments: This work was supported by the MSIT, Korea, under the ICT Consilience Creative program (IITP-2019-2011-1-00783), the Basic Science Research Program through the NRF funded by the MSIT (NRF-2017R1A5A1015596), and the POSCO Green Science Project funded by POSCO, Korea.
INDIVIDUAL DAILY CARBOHYDRATE INTAKE IS INVERSELY ASSOCIATED WITH GLYCAEMIC CONTROL IN ADULTS WITH TYPE 1 DIABETES USING A HYBRID CLOSED-LOOP SYSTEM
Abstract
Background and Aims
With the clinical implementation of hybrid closed-loop (HCL) systems, efforts are moving towards personalised medicine. However, sparse evidence exists on how individual carbohydrate (CHO) intake affects glycaemic control in type 1 diabetes (T1D). The HCL-device MiniMed 670G requires CHO-input for meal-time bolus calculation while in “auto-mode”. We aimed at assessing glycaemic control as a function of individual daily CHO-intake.
Methods
Between 11/2018 and 06/2019, we evaluated CHO-intake (g/day) and CGM data in adults with T1D using the MiniMed 670G system at our tertiary referral centre. Mean individual daily CHO-intake (MIDC) was assessed for each participant. For each day, the relative deviation from MIDC (rMIDC) was calculated, and days were stratified into low, medium and high CHO-days (≤80%, 81–120% and >120% rMIDC, respectively). CGM read-outs were used to calculate time in target range (TIR, 3.9-10.0 mmol/l), time above target range, and time below target range.
Results
We included 21 patients with T1D (11 male, 10 female; age 39.2±14.7y; HbA1c 7.0±0.9%) providing a total of 879 days of data (mean 42.0±39.2d per patient, 9-186d). Mean individual time in auto-mode was 97.5±4.7%. Time in target range (TIR) for the low, medium and high CHO-days was 82.1±13.9%, 79.2±14.9% and 75.8±14.6%, respectively (p<0.001). Time above target range was 15.8±13.1%, 18.8±14.3% and 22.6±14.7%, respectively (p<0.001). There was no significant difference for time below target range.
Conclusions
Individual daily CHO-intake was inversely associated with glycaemic control in adults with T1D using the MiniMed 670G HCL-system, corroborating the importance of personalised treatment recommendations.
COMPARISON OF TWO PREGNANCIES OF A WOMAN WITH TYPE 1 DIABETES WITHOUT AND WITH AAPS (ANDROID ARTIFICIAL PANCREAS SYSTEM) SUPPORT
Abstract
Background and Aims
The tight metabolism targets of women with type 1 diabetes (T1D) during pregnancy are associated with a high frequency of hypoglycaemia which impose a significant burden on these women’s lives. Currently no commercial artificial pancreas system (APS), that could mitigate this burden, is approved during pregnancy.
Methods
A woman with 30 years of T1D underwent two subsequent pregnancies: Pregnancy one at age 35 using multiple daily injections (MDI) therapy (insulin glargine, Sanofi and insulin lispro, Eli-Lilly) with flash glucose monitoring (FGM; Abbott Libre Flash). Pregnancy 2 at age 37 using OpenAPS software algorithm in combination with established hardware (AC Combo, Roche Diabetes Care and Dexcom G5, Dexcom) using insulin (lispro, ELI-Lilly). Data on HbA1c, the woman’s hypoglycaemia perception, maternal weight development during the pregnancy, insulin doses (before, during and after pregnancy), childbirths, complications and birth weight of the children were collected from medical records, mother-child-passes and Nightscout downloads. Data were retrospectively analysed.
Results
No differences in above 6 of the 7 mentioned parameters were found. However, the first pregnancy with MDI and FGM showed severe hypoglycaemias, while in the second one (AAPS) no severe hypoglycaemia or hypoglycaemia unawareness occurred.
Conclusions
AAPS in pregnant women with T1D can improve metabolic control at reduced risk of hypoglycaemia leading to substantially improved quality of life. Pregnant women with T1D are not willing to wait for commercially available closed loop systems.
HYBRID CLOSED LOOP AND ALGORITHMS IMPROVE METABOLIC CONTROL IN TYPE 1 DIABETIC PATIENTS.
Abstract
Background and Aims
Predictive low-glucose suspend (PLGS) insulin delivery system and hybrid closed loop (HCL) systems may improve glucose control in type 1 diabetic individuals. This is a single-center, retrospective, observational study to evaluate the effect on metabolic control and glucose variability of PLGS and HCL systems compared to sensor-augmented pump (SAP) therapy.
Methods
We retrospectively analyzed seventy-nine adults with type 1 diabetes on insulin pump therapy, matched for age, gender and BMI. The mean follow-up was 3.5±1.9 years.
Results
Forty patients (mean age 51,2±16,1 years, F/M 19/21), who are in treatment with HCL system (Minimed 670G, Medtronic, Northridge, CA) or with PLGS feature (Minimed 640G, Medtronic, Northridge, CA) (Group 1), were compared to 39 subjects in SAP therapy (mean age 47,8±10,5 years, F/M 15/24) (Group 2). Group 1, compared to Group 2, showed lower HbA1c levels (7.2±0.8% vs 7.6±0.9%, p=0.07), and a statistically significant higher percentage of time that interstitial glucose level was within the target range, defined as 70 to 180 mg per deciliter (65.3±12.4% versus 56.1±16.4%, p=0.03). Moreover, Group 1 showed a significant lower time spent in hypoglycemic range compared to Group 2 (2.0±1.7% versus 6.7±5.6%, p=0.001).
Conclusions
PLGS and HCL systems were more effective in improving glucose control and in reducing the risk of hypoglycaemia in patients with type 1 diabetes, thereby mitigating risk for acute and chronic complications.
ACCURACY ANALYSIS OF AN AUTONOMOUS SYSTEM TO PERSONALIZE BLOOD GLUCOSE PREDICTION FOR T1DM PATIENTS WITH REAL WORLD DATA
Abstract
Background and Aims
BGL predictive algorithms can improve T1DM treatment preventing glucose excursions. An autonomous system based on neural networks was developed to personalize blood glucose predictions based on blood glucose, insulin infusion, nutrient intakes and heart rates in a real world scenario.
Methods
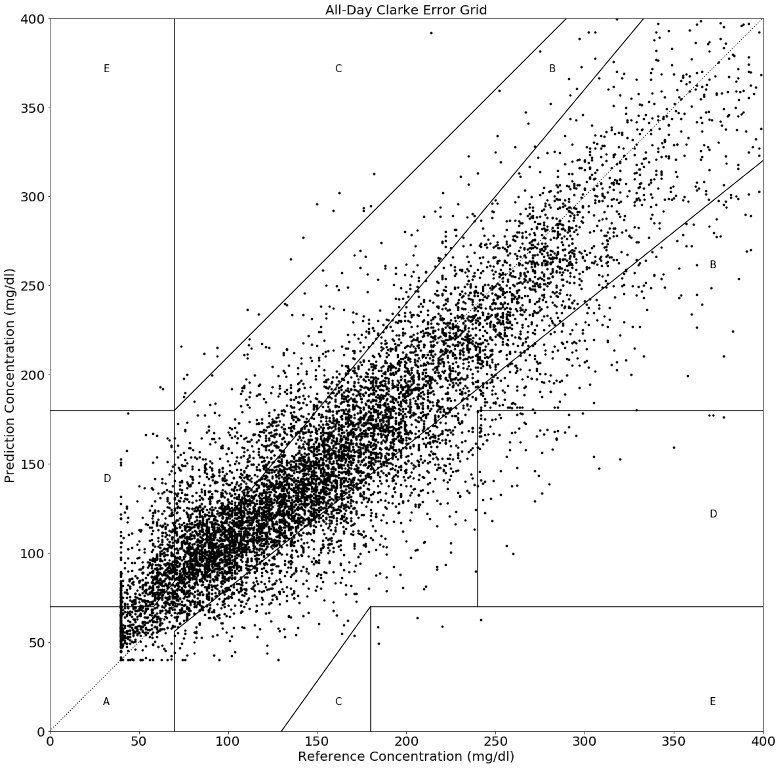
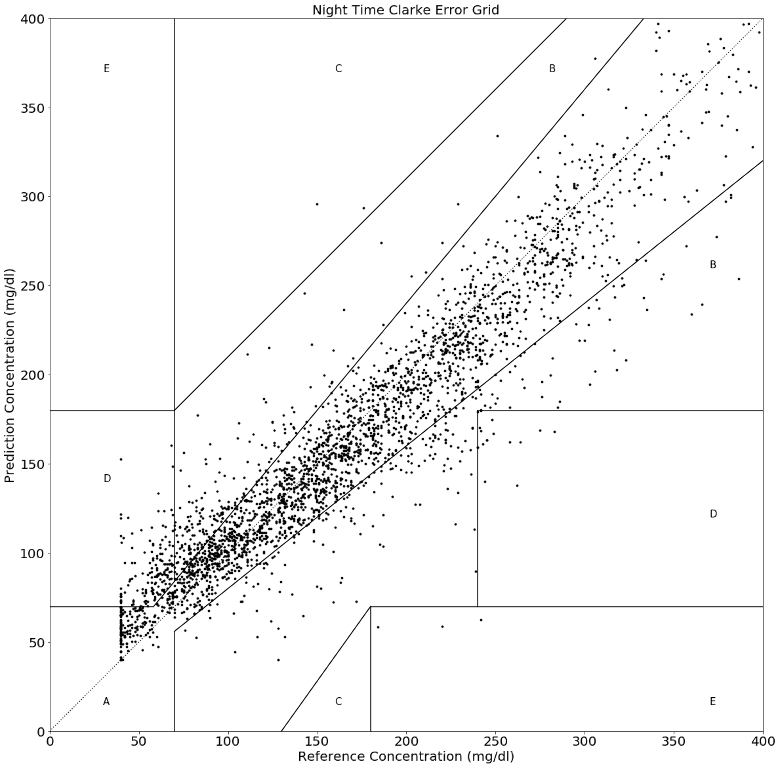
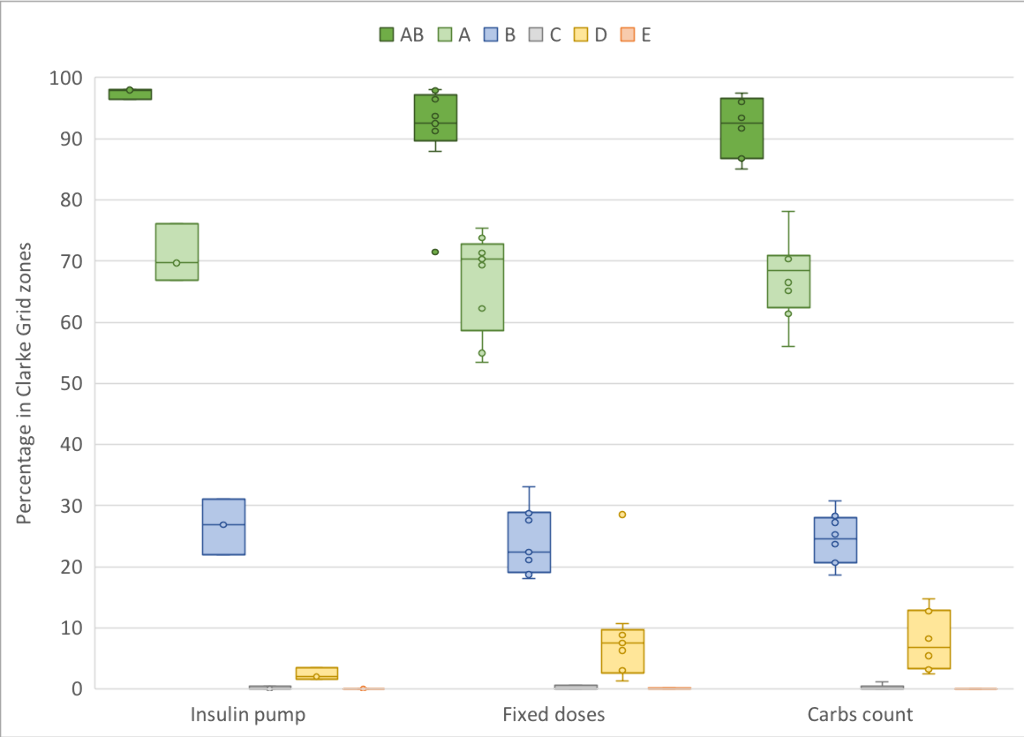
20 T1DM patients were monitored with flash glucose monitor, activity tracker and mobile app (GlucoTrends) to collect meal and insulin data. Personalized prediction models were trained independently, without requiring specific settings for each individual. Patient's characteristics: 9 female, age: 32.4(SD:10.5), BMI: 26.0(3.8), BGL: 159.1(34.0), under the following therapies: 45% under fixed doses, 40% carbohydrate-count and 15% insulin pumps. Patients were monitored during on average 29.3 days (SD: 7.9), and the last 20% measurements were reserved for evaluation. Prediction accuracy for 1-hour prediction horizon was evaluated by Clarke Error Grid (CEG) compareding to BGL measured with flash monitor.
Results
The percentage of predictions within AB zones of CEG for all-day and only for night-time periods are 92.9% and 94.0%, respectively (Figure 1). Patients using Insulin Pumps, Analog insulin and Human insulin had 97.5%(0.7), 93.6%(4.5) and 90.0%(8.2) predictions within AB zone on average, respectively.
Conclusions
Our proposed algorithm has demonstrated to be capable to personalize glucose prediction in a real world scenario and poses as a potential solution for an autonomous support system. In our study different insulin regimen and molecules confirmed expected results. Higher than desired predictions in zone D may be caused by sensor's error biases within minimum glucose levels.
TOWARD A PERSONALIZED DECISION SUPPORT SYSTEM FOR BLOOD GLUCOSE MANAGEMENT DURING AND AFTER PHYSICAL ACTIVITIES IN PATIENTS WITH TYPE 1 DIABETES
Abstract
Background and Aims
Physical activities have a significant impact on blood glucose homeostasis of patients with type 1 diabetes. The risk of hypoglycemia (low blood glucose) is significantly higher during and after physical activities, especially for individuals who experience hypoglycemia unawareness. Our research aims to reduce the risk of hypoglycemia and empower type 1 diabetes patients in making decisions regarding food choices, insulin, exercise intensities and other factors in connection with physical activities.
Methods
Using historical physical activity data, a feedforward neural network is trained to provide a prediction of the blood glucose outcome during and after physical activities. Based on the personalized neural network and Q learning (a model free reinforcement learning), optimal actions that minimize the risk of hypoglycemia and improve blood glucose regulation are provided to the patient.
Results
In-silico results on a blood glucose simulator with the Breton’s physical activity model show that the proposed methodology is capable of maintaining the blood glucose in the healthy range during and after physical activities. No hypoglycemia has occured when following the recommendation of the decision support system.
Conclusions
The research shows the potential of using machine learning in reducing the risk of hypoglycemia and better glycemic control during and after physical activities. Important research are identified and conducted to reduce the roller coaster effect and provide better combination of food intake, insulin and other factors for patients in their daily management of type 1 diabetes.
BLOOD GLUCOSE PREDICTION WITH A FRACTIONAL ORDER NEURAL NETWORK
Abstract
Background and Aims
Blood Glucose (BG) prediction models need to be improved to ameliorate BG regulation. Neural Networks (NN) and fractional order calculus are powerful tools for black box modeling. This work combines both approaches to propose the first NN model with fractional order learning algorithm to improve BG prediction.
Methods
The NN model (Fig. 1A), which uses BG, Insulin on board, and carbohydrates on board as inputs, consists of a three-layer NN with 2-2-1 neurons in the input, hidden and output layers, respectively. The NN was trained by a learning algorithm using the Grünwald-Letnikov fractional derivative (2).
Evaluation is performed on 10 T1D patients (aged > 18 years). Training is performed using 10 days of data and test is performed using 5 days of data unseen by the NN during training. RMSE is computed to evaluate accuracy on BG prediction 30-, and 60-min-ahead.
Results
Table 1 displays results reached by the proposed model and results reported in the literature. Fig. 1B shows RMSE reached by the proposed NN-based model on the 10 validation subsets (10 patients, 5 days). As expected, RMSE ± std increases when prediction horizon increases.
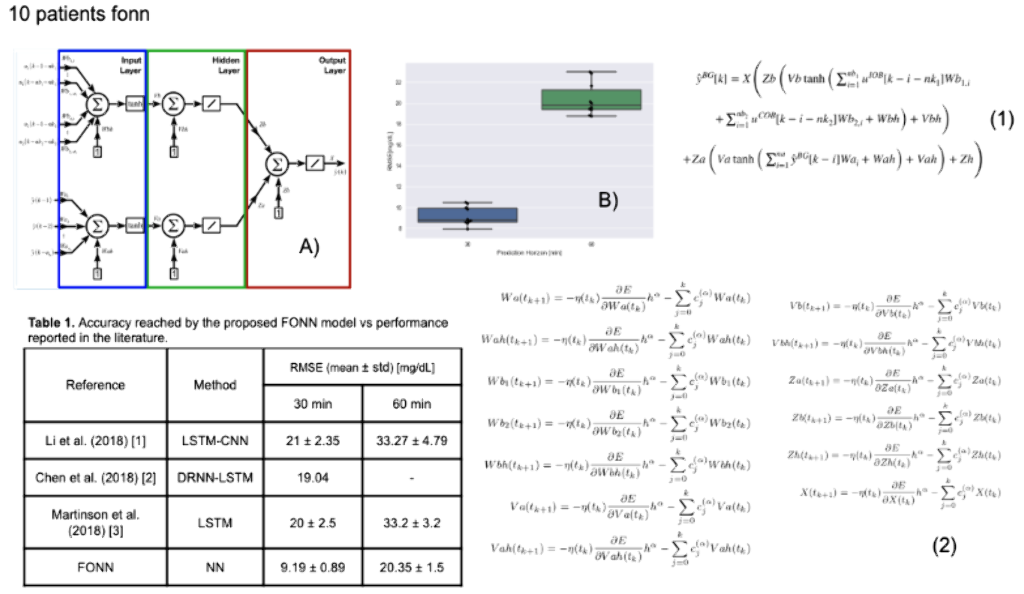
Conclusions
This work presented a NN-based BG prediction model trained by a fractional order learning algorithm. The proposed model reached the best performance on predictions 30- and 60-min-ahead, compared with results reported in the literature. Furthemore, the proposed model is the simplest of the compared approaches. In future works, the possibility to predict hypo- and hyperglycemia events by the proposed model will be evaluated.
SIMPLIFYING THE MEAL-TIME BOLUS CALCULATION: ACCURACY OF A PERSONALIZED SMALL/MEDIUM/LARGE (S/M/L) OPTION
Abstract
Background and Aims
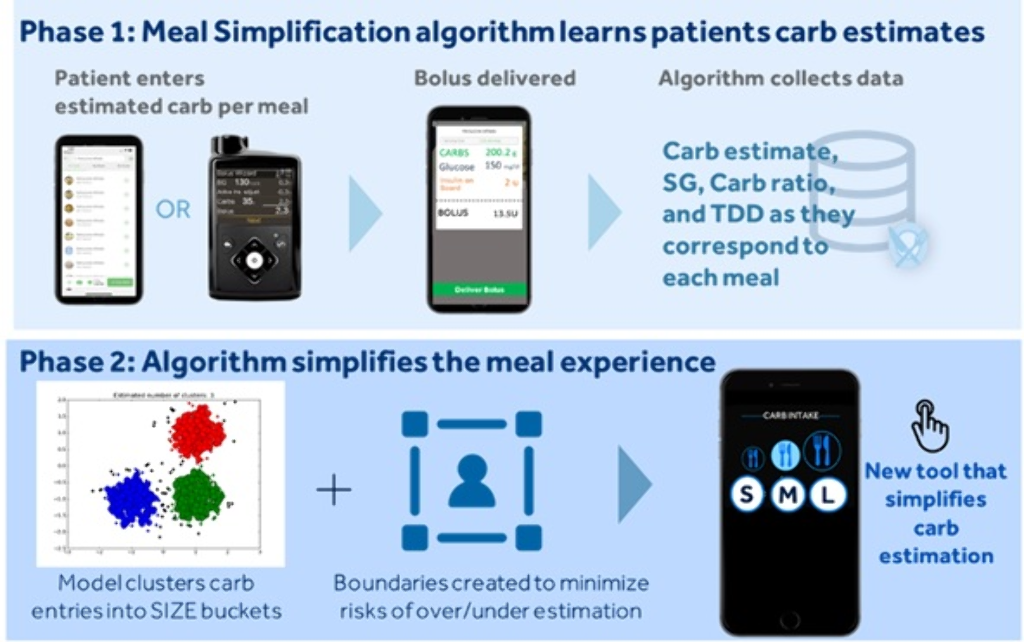
To simplify the complexity of carb counting, a Meal Simplification (MS) algorithm was developed that allows one to choose a user-specific small, medium, or large carb-entry size (S/M/L), instead of entering estimated carbs to the nearest gram.
Methods
The MS system works in two phases (Figure). Phase-1 is the learning phase where traditional carb-counting and entry are carried out via insulin pump or app. Once enough data are collected and uploaded to the cloud, the system enters Phase-2 where it uses machine-learning techniques to identify clusters of meals based on meal size. A set of common S/M/L meal sizes with a corresponding range of carb values and a centroid carb value, on which a meal bolus amount is calculated, is determined. The user has the option to override the centroid carb value to adjust for the actual size of a specific meal. The algorithm updates the S/M/L carb-entry sizes to accommodate for these changes. An in-silico experiment was conducted with 2087 virtual Type 1 Diabetes subjects using the Medtronic Advanced Hybrid Closed-loop system.
Results
For mealtime boluses, the Control group involved the traditional carb-counting method. The Intervention group involved personalized S/M/L meal-clustering. Time spent between 70-180 mg/dL, <70 mg/dL, >180 mg/dL, and >250 mg/dL for the Control versus Intervention arm were 85.1±6.8% versus 84.5±6.6%, 2.0±2.6% versus 2.1±2.5%, 12.9±7.1% versus 13.4±7.1%, and 2.1±2.1% versus 2.3±2.6%, respectively.
Conclusions
Personalized Meal Simplification algorithms for pump users are expected to reduce the burden of carb counting to the nearest gram, without increasing hypoglycemia/hyperglycemia exposure.
COST EFFECTIVENESS ANALYSIS OF MINIMEDTM 670G SYSTEM VERSUS CONTINUOUS SUBCUTANEOUS INSULIN INFUSION, IN INDIVIDUALS WITH TYPE1 DIABETES IN THE UNITED KINGDOM
Abstract
Background and Aims
This study assesses the long-term cost-effectiveness of the MiniMedTM 670G hybrid closed loop system versus Continuous Subcutaneous Insulin Infusion (CSII) alone in people with type 1 diabetes (T1D) in UK.
Methods
The IQVIA-CORE-Diabetes-Model was used to perform cost-effectiveness analysis over patient lifetime. Clinical data were sourced from pivotal clinical study comparing MiniMedTM 670G system with CSII in people with T1D; in which the use of MiniMedTM 670G system was associated with a reduction in HbA1c of 0.5% (5.5 mmol/mol), from 7.4% (57 mmol/mol) at baseline to 6.9% (52 mmol/mol) at the end of the study. Cost data, expressed in 2018 British pounds (GBP), were obtained from UK reference-prices and the published literature.
Results
The MiniMedTM 670G system was associated with a quality-adjusted life-year (QALY) gain of 1.74 but higher overall costs versus CSII, leading to an incremental cost-effectiveness ratio (ICER) of GBP 20,421 per QALY gained. Use of MiniMedTM 670G system resulted in a lower cumulative incidence of diabetes-related complications. Higher MiniMedTM 670G system acquisition costs were partially offset by reduced complication costs. In patients with HbA1c≥7.5% at baseline, MiniMedTM 670G system was associated with 2.02 incremental QALYs versus CSII, yielding an ICER of GBP12,892 per QALY gained. Extensive sensitivity analysis on key drivers confirmed the robustness of results.
Conclusions
The MiniMedTM 670G system was associated with clinical benefits and quality of life improvements in people with T1D relative to CSII. At a willingness-to-pay threshold of GBP20,000 per QALY-gained, MiniMedTM 670G System likely represents a cost-effective treatment option for people with T1D in UK.
EFFECTIVENESS AND SAFETY OF A HYBRID CLOSED LOOP SYSTEM IN CHILDREN AND ADOLESCENTS WITH TYPE 1 DIABETES: 1-YEAR EVALUATION.
Abstract
Background and Aims
We evaluated the efficacy and safety of a hybrid closed loop (HCL) system after its arrive in Italian market in October 2018 and during 1-year follow-up.
Methods
We prospectively analyzed data of all patients who started the Minimed 670G system, (Medtronic, CA, USA) after 1 year since its arrival. Main outcome is the time in range (TIR). Secondary outcomes are HbA1c change from baseline, time in hypo (70-54 and <54), time in hyper (>180 mg/dl and >250), coefficient of variation (CV).
Results
After 1-year follow-up, 52 patients (mean age 11±5 yr s, range 6-20 yrs, diabetes duration 7±4 yrs) had a TIR of 71.3±17.6% when considering 70-180 mg/dl (range 32-97%), using the system in automatic mode for 84% of time. HbA1c significantly improved (7.12±0.87 vs 7.62±1.7, p=0.001). Time in hypo, in hyper and CV were respectively 1.8±1.9%, 0.63±1.0%, 18.2±8.0, 8.0 ±11.3 and 33±5.7% (n.v. <36%). A significant correlation has been observed between TIR and time in automatic mode (r=0.891, p=0.001). Considering the patients using the system >70% in automatic mode (n=42, 81%), TIR was 80.9±7.6%, using the system in automatic mode for 93% of time. Time in hypo, in hyper and CV were respectively 2±2.1%, 0.7±1.1%, 14.3±5.7, 2.1 ±1.4 and 31±5 %
Conclusions
670G system is effective to achieve a high TIR. A systematic educational pathway, as the one used by 640G users, could help reach recommended target even in pediatric population, overcoming some constrains observed using 670G system. A decalogue to help users will be proposed.
CONTROL AND ESTIMATION OF DIABETES MELLITUS BY ROBUST FIXED POINT TRANSFORMATION METHOD
PERFORMANCE OF OMNIPOD PERSONALIZED MODEL PREDICTIVE CONTROL ALGORITHM WITH MULTIPLE SETPOINTS AND MEAL AND EXERCISE CHALLENGES IN CHILDREN AGED 2-12 YEARS WITH TYPE 1 DIABETES
- Jennifer Sherr, United States of America
- Bruce A. Buckingham, United States of America
- Gregory P. Forlenza, United States of America
- Alfonso Galderisi, United States of America
- Laya Ekhlaspour, United States of America
- R. Paul Wadwa, United States of America
- Melinda Zgorski, United States of America
- Ryan Kingman, United States of America
- Cari Berget, United States of America
- Joon Bok Lee, United States of America
- Jason O’connor, United States of America
- Bonnie Dumais, United States of America
- Todd Vienneau, United States of America
- Lauren Huyett, United States of America
- Trang Ly, United States of America
Abstract
Background and Aims
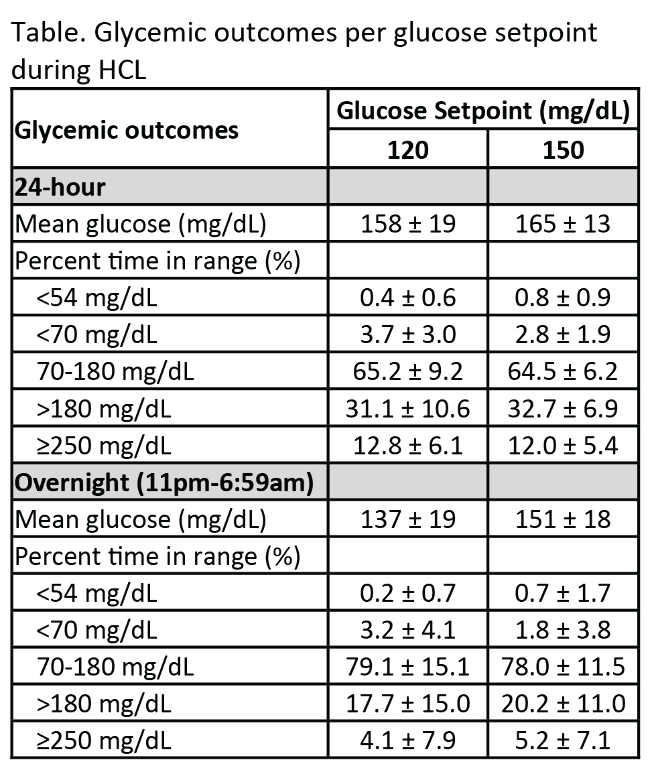
The Omnipod hybrid closed-loop (HCL) personalized model predictive control (MPC) algorithm was assessed in children aged 2-12y with type 1 diabetes (T1D) using an investigational device. This study provided the first evaluation at multiple glucose setpoints and with missed meal boluses in this age group.
Methods
Participants aged 2-12y with T1D and A1C<10.0% using CSII or MDI were eligible for a 72-96-h HCL study conducted in a supervised free-living hotel setting. At HCL start, the glucose setpoint was 150mg/dL, and at 24-48h it was lowered to 120mg/dL. The system was stress-tested with 1-2 missed lunch boluses, high fat dinners, and daily moderate-intensity exercise. Endpoints were mean glucose and percentage time <54, <70, 70-180, >180, and ≥250mg/dL at each setpoint.
Results
Participants (n=9) were (mean±SD): age 7.1±2.2y, T1D duration 3.0±1.6y, and A1C 7.6±1.0%. Glycemic outcomes at each setpoint are reported in the Table. Despite stress-testing the system with missed meal bolus challenges (20-75g carbohydrate) and exercise, percentage time in target range (TIR) from 70-180 mg/dL was ~65% regardless of the system setpoint. Mean glucose was 158±19mg/dL and 165±13mg/dL at the 120mg/dL and 150mg/dL setpoints, respectively.
Conclusions
The Omnipod personalized MPC algorithm performed well and was safe for up to 5 days of use in children aged 2-12y with T1D when stress-tested at 2 different setpoints under challenging conditions. With recent consensus guidelines recommending TIR >60% for youth, our data demonstrate the feasibility of attaining this goal despite the challenges imposed in this trial.
NIGHT TIME GLYCEMIC CONTROL BEFORE AND AFTER MINIMED™ 670G SYSTEM USE BY CHILDREN WITH T1D 2-6 YEARS OF AGE
Abstract
Background and Aims
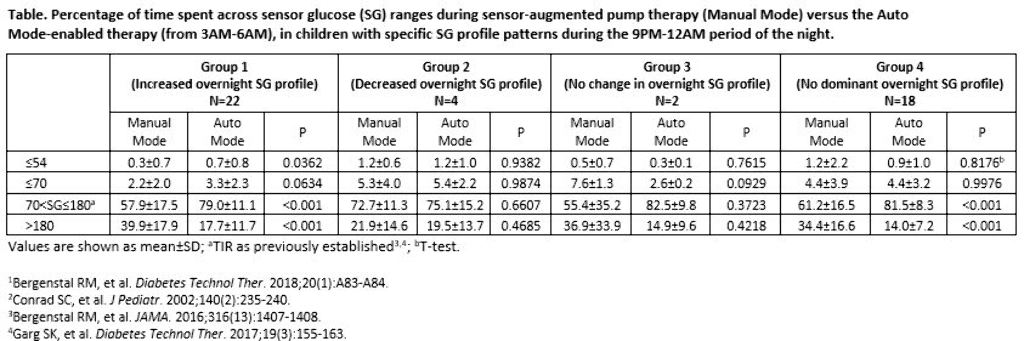
Adults who experienced increased overnight glucose variability or insulin delivery needs (akin to dawn phenomenon) during the MiniMed™ 670G system trial baseline run-in, exhibited improved overnight glycemic control after three months of Auto Mode use.1 The impact of Auto Mode use on the overnight glycemia of the youngest pediatric cohort of the MiniMed™ 670G system trials was investigated.
Methods
The 9PM-12AM sensor glucose (SG) profile of participants aged 2-6 years with T1D was analyzed, based on Conrad et al. 2002.2 Profiles were categorized as displaying a 1) >10 mg/dL increase in SG, 2) >10 mg/dL decrease in SG, or 3) No change in SG (≤10 mg/dL decrease or increase) and for >50% of the two-week baseline. If an SG profile did not present with an aforementioned pattern, it was categorized into a fourth group (No dominant SG profile). The percentage of early morning (3AM-6AM) time spent across SG levels were compared.
Results
There were 22, 4, 2, and 18 participants in Groups 1, 2, 3, and 4, respectively, during baseline. After three months of Auto Mode use, participants numbered 11, 1, 1, and 33, respectively. Significantly improved time in target glucose range (TIR, >70-180 mg/dL) was observed in Groups 1 and 4. Time spent at ≤70 mg/dL increased for Group 1, but was not significant.
Conclusions
Children with T1D displayed different profiles of overnight SG variability during the MiniMed™ 670G system trial. Regardless of the varied profile patterns observed, the MiniMed™ 670G system safely and effectively improved or did not change overnight TIR.
DEVELOPMENT PLATFORM FOR ARTIFICIAL PANCREAS ALGORITHMS
Abstract
Background and Aims
Assessing algorithms of artificial pancreas systems is critical in developing automated and fault-tolerant solutions that work outside clinical settings. The development and evaluation of algorithms can be facilitated with a platform that conducts virtual clinical trials. We present a clinically validated cloud-based distributed platform that supports the development and comprehensive testing of single and dual-hormone algorithms for type 1 diabetes.
Methods
The platform is built on principles of object-oriented design, and runs user algorithms in real-time virtual clinical trials utilizing a multi-threaded environment enabled by concurrent execution over a cloud infrastructure. Users import a plugin into their algorithms (Matlab, Python, or Java) to connect to the platform. Once connected, users interact with a graphical interface to design experimental protocols for their trials. Protocols include trial duration in days, meal times and amounts, variability in meal times and amounts, carbohydrate counting errors, snacks, and onboard insulin levels. We validate and integrate into the platform a glucoregulatory system of ordinary differential equations (ODEs) parameterized with clinical data to mimic the inter and intra-day variability of glucose responses of 15 T1DM patients.
Results
The platform facilitates development by solving the ODE model in the cloud on large CPU-optimized machines, providing a 50% improvement in memory, speed and CPU utilization. Users can easily debug & modify code, test multiple strategies, and generate detailed clinical performance reports.
Conclusions
The platform utilizes the validated patient model to conduct virtual clinical trials for the rapid development and testing of closed-loop algorithms for T1DM.
REAL-WORLD VARIATION IN SENSOR GLUCOSE RESPONSE TO SIMILAR CARBOHYDRATE AND INSULIN
Abstract
Background and Aims
Most insulin bolus calculators model carbohydrates, insulin, and the rise in sensor glucose(SG) as a linear relationship, which does not account for meal-to-meal variations in insulin sensitivity, glycemic index, or nutrient content. The variation between carbohydrates, insulin, and SG level was evaluated in a population of real-world individuals using a sensor-augmented pump(SAP) to manage diabetes.
Methods
Data from 1825 SAP system users were voluntarily uploaded to CareLink™ Personal between January 2014 and October 2018 and retrospectively analyzed if ≥20 valid meals were logged. Glucose response to insulin and carbohydrates taken with a meal were measured using the Sensor Glucose Response Metric(SGRM) calculated as (SGΔ+Insulin*ISF)/Carbohydrate. SGΔ is the change in SG level from meal start to the first SG level peak. Insulin Sensitivity Factor(ISF) is the estimated glucose-to-insulin response(mg dL-1/unit). The variance in SGRM between meals users, and time of day was also determined.
Results
The mean±SD of meals for the 1825 users was 221±390. 402,941 meals were analyzed. The mean±SD of the SGRM across users was 8.4±4.3mgdL-1/gram and the average intra-user SD was 5.7mgdL-1/gram. The SGRM mean and standard deviation decreased from 3am-9pm. However, intra-user SGRM SD hit a max of 5.4mgdL-1/gram from 6am-9am.
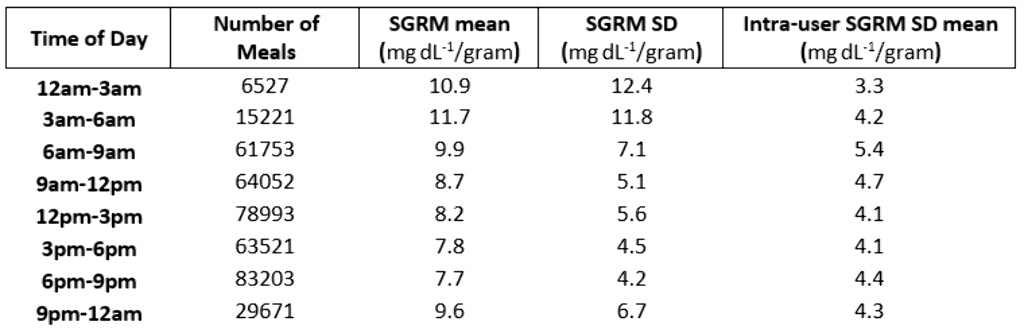
Conclusions
The calculated SGRM of SAP therapy users revealed the potential impact of metabolic and meal-component factors(e.g., glycemic index, nutrient content, time of day, and other contextual factors) that influence glucose response in a non-linear fashion. These preliminary findings, on factors outside of carbohydrate and insulin, build toward the development of more advanced automated insulin delivery and predictive CGM systems.
DEEP REINFORCEMENT LEARNING IN THE PREDICTION OF BLOOD GLUCOSE
Abstract
Background and Aims
If individuals with diabetes want to be able to take measures in anticipation of forthcoming hypo- and hyperglycaemic events, it is essential to predict future blood glucose levels. We now report the first application of deep reinforcement learning to improve prediction of blood glucose made by a pre-trained deep neural network based on long-short term memory (LSTM).
Methods
In support of a pre-trained LSTM sequential model, an adjustment module based on Double Deep Q-Learning (DDQN) was introduced to fine tune the prediction of blood glucose. The algorithm was trained and tested on retrospectively collected data from 6 real-patient (OhioT1DM Datasets). Both LSTM and DDQN models use 4 history glucose data (look-back, sampling time 5 minutes); the former predicts a “basic” glucose value for a prediction horizon of 30 minutes, and the latter adjust, if needed, the “basic” prediction.
Results
As shown in Table 1, the DDQN model improved the performance of the LSTM sequential model. The Time Lags were decreased - without obvious influence on the Root Mean Square Error or the Correlation Coefficient (CC).
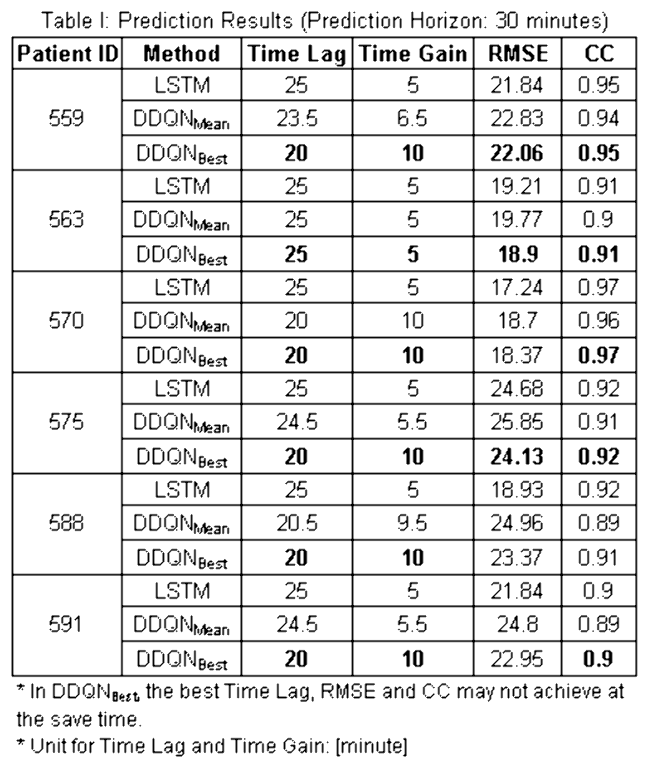
Conclusions
A deep reinforcement learning algorithm has been introduced to enhance the performance of a pre-trained deep LSTM network in predicting blood glucose. The preliminary results are promising, especially with respect to the delay between predicted value and real data.
EVALUATING REWARD FUNCTIONS FOR BLOOD GLUCOSE CONTROL USING REINFORCEMENT LEARNING IN THE ARTIFICIAL PANCREAS
Abstract
Background and Aims
Reinforcement learning (RL) is a promising option for adaptive and personalized algorithms for the artificial pancreas. However, when adapting reinforcement learning algorithms to new domains where a natural reward function is not given directly, such as in the T1DM case, suitable reward functions have to be crafted by hand. This design process is susceptible to errors and is in fact a general open area of research within RL.
In this work we train a single RL agent using several different reward functions in the hybrid closed loop setting. We evaluate both generic and domain-knowledge based rewards functions.
Methods
We test eight different reward functions in-silico on the Hovorka simulator. The reinforcement learning agent is trained using Trust-Region Policy Optimization (TRPO), a policy gradient algorithm that has shown previous competitive performance controlling blood glucose level in T1DM.
Performance is measured in terms of the average reward of the algorithms as well as average time in-range, -hypo and -hyper. A total of 100 days with randomized meals and fixed seed are used for generating the test averages.
Results
We test the algorithm on episodes lasting one and a half day containing four randomized meals and simulated carbohydrate counting errors. Figure 1 shows an example comparing two different reward functions - a Gaussian reward function and an asymmetric function designed to spend less time in hypoglycemia.
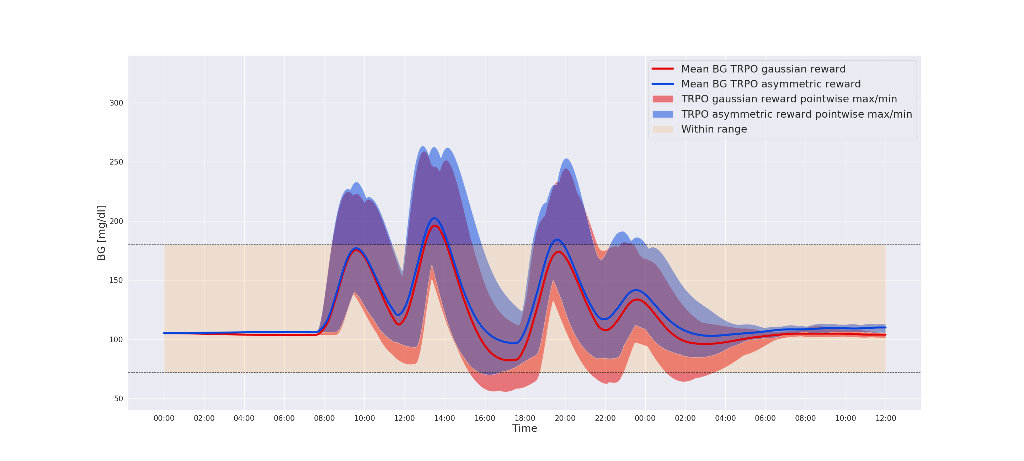
Conclusions
Our in-silico experiments shows that by tuning the reward function using domain specific knowledge of T1DM, we are able to avoid hypoglycemic events while increasing overall time-in-range.
THE USABILITY OF A HYBRID CLOSED-LOOP INSULIN DELIVERY SYSTEM: SIMULATED USE STUDIES OF THE TANDEM T:SLIM X2 INSULIN PUMP WITH CONTROL-IQ TECHNOLOGY
Abstract
Background and Aims
Advanced hybrid closed-loop (HCL) insulin delivery systems are being developed and used to minimize fluctuations in blood glucose levels associated with insulin therapy in people with diabetes. Usability of these systems is critical for their effectiveness.
The objective was to assess the usability and safety of a touchscreen, wearable insulin pump with an operating system that automatically adjusts insulin delivery based on a) predicted continuous glucose monitor (CGM) readings and b) user input that informs the pump of food intake and activity levels.
Methods
70 participants, composed of insulin pump users and MDI users, completed the usability studies. The participants were given real-life scenarios as context for simulated use tasks and knowledge tests. Tasks and tests were designed to assess the safety and ease of use of a Tandem t:slim X2 pump designed with a HCL insulin delivery system. Task success rates were collected, and a Systems Usability Scale (SUS) questionnaire was administered at the end of each session.
The formative study gave its 10 adult pump users a 10-minute orientation to the system. The summative study gave its 60 pump and MDI users real-world training, with a decay period before testing.
Results
The average SUS scores were identical at 84 indicating a high user satisfaction (typical scores 65-75). Task completion rates of 93% and 96% were observed, respectively.
Conclusions
The findings indicate that the Tandem t:slim X2 insulin pump with a hybrid closed-loop (HCL) insulin delivery system was both intuitive and safe to use.
ESTIMATION OF INSULIN ASPART AND LISPRO PEAK ACTION TIME AT POPULATION AND INDIVIDUAL LEVELS FROM INSULINEMIA MEASUREMENTS OF TYPE 1 DIABETIC PATIENTS
Abstract
Background and Aims
Insulin aspart and lispro are common analogs with a guide peak time of 1 to 3 hours. In practice, insulin action speed varies depending on formulation and patient metabolism.
In an artificial pancreas, the predicted glycaemia accuracy relies on the kinetic model of insulin subcutaneous diffusion. We aim to estimate the peak time for both analogs from insulinemia measurements Im(t).
Methods
First, the Insulin On Board (IOB) is modelled with Hovorka’s set of two sub-compartments and output plasma insulin I(t). We estimate the model’s parameters tmax, Vi and ke by minimising the quadratic error between Im(t) and I(t). The reference IOBref is equal to the sum of sub-compartments.
Then, the IOB is modelled with an exponential function IOBexp, decreasing with time and depending on τ. The optimal τ minimises the quadratic error between IOBexp(t,τ) and IOBref for all patients at once.
Results
During 24h at hospital, 41 patients with type 1 diabetes, including 20 using aspart and 21 using lispro, were monitored during clinical trials Diabeloop-SP3 and SP6.1. Measurements include CGM, basal, bolus and insulinemia Im(t).
The median individual tmax was estimated at 57 min [Q1: 49; Q3: 64] for aspart and 53 min [43; 57] for lispro. The population-optimal τ is 62 min for aspart, and 65 min for lispro.
Conclusions
In this study, insulin aspart and lispro peak times were estimated at both individual and population levels. Such values are essential to improve the glycaemia prediction accuracy by an artificial pancreas and to achieve a better diabetes management.
INVESTIGATING EFFECTS OF INSULIN ESTIMATION ON FUTURE INSULIN SENSORS’ DESIGN AND IMPLICATION FOR DIABETES MANAGEMENT
- Varuni Sarwal, United States of America
- Kelilah L. Wolkowicz, United States of America
- Sunil Deshpande, United States of America
- Joseph Wang, United States of America
- Jordan E. Pinsker, United States of America
- Lori Laffel, United States of America
- Mary-Elizabeth Patti, United States of America
- Francis Doyle III, United States of America
- Eyal Dassau, United States of America
Abstract
Background and Aims
Incorporation of an insulin sensor may help to improve performance of future AP algorithms by reducing severe hypoglycemic events. Optimal insulin measurement intervals were identified for a feedback-based threshold suspend safety-layer.
Methods
Personalized Kalman filter-estimated plasma insulin concentration (EPIC) measurements were used to supplement a zone model predictive control algorithm. Insulin delivery was suspended when both CGM was <140 mg/dL and EPIC values were greater than a personalized threshold based on fasting basal insulin concentrations. EPIC measurements occurred at 5-, 30-, 60-, 120-, and 180-minute intervals. Using the UVA/Padova Simulator, the controller was evaluated across ten in-silico subjects for three 8-hour, 50-gram carbohydrate scenarios: 1) sixty-minute exercise, induced via increasing glucose uptake rates, one hour after an announced meal, 2) meal size overestimation by 35% with carbohydrate ratio underestimated by 25%, and 3) announced meal (baseline).
Results
Implementing the EPIC safety-layer, the mean percent time below 70 mg/dL decreased: from 8.09±9.08% to 2.47±5.24% for 5-minute, 7.07±7.75% for 30-minute, 7.57±8.28% for 60-minute, and 7.59±8.26% for 120- through 180-minute intervals (scenario 1); from 5.07±5.33% to 0.00±0.00% for 5- through 30-minute, 0.87±2.76% for 60-minute, 2.12±4.65% for 120-minute, and 3.16±5.38% for 180-minute intervals (scenario 2); and from 0.69±2.17% to 0.00±0.00% for 30- through 120-minute, while remaining at 0.69±2.17% for 180-minute intervals (scenario 3). Infrequent measurements of 30- to 120- minutes resulted in slight performance degradation with increasing sample time.
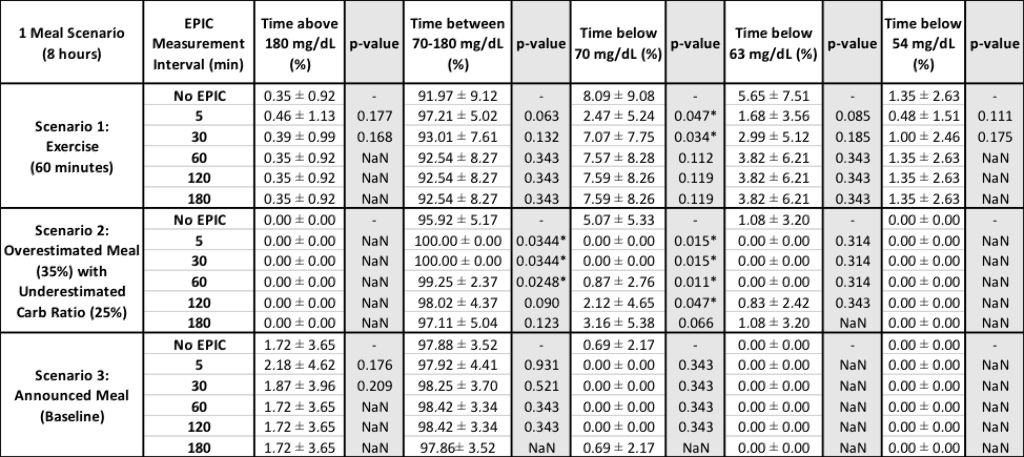
*Indicates p-value<0.05
Conclusions
The EPIC safety-layer in-silico prevented severe hypoglycemia during challenging scenarios without significant rebound hyperglycemia. Future insulin sensors could potentially be designed utilizing 30- to 120-minute measurement intervals.
A NOVEL SIMULATION ENVIRONMENT MODELING REALISTIC INTERACTIONS BETWEEN PATIENTS AND DECISION SUPPORT SYSTEMS
Abstract
Background and Aims
Diabetes self-management requires high cognitive effort and many daily actions by patients. Decision support systems (DSS) can simplify this process. However, integration of connected devices increases system complexity, justifying the need of dedicated development tools. Existing physiological simulators support the design of closed loop control algorithms but lack description of user-device interaction especially in non-closed-loop settings. Here we present a simulation approach designed to support the development of DSS with increasing complexity.
Methods
To describe realistic behavior, we integrated domain knowledge of device characteristics, patient behavior and environmental factors. By making use of probabilistic modeling techniques, simulation is not limited to pre-defined situations but covers a wider range of alternative scenarios.
Results
We developed a modular simulation environment that allows a holistic description of diabetes therapy self-management as the interactions between the patient, devices, DSS and the environment. We relied on qualitative research to describe therapy tasks as a series of atomic actions. Each task was modelled using Markov chains. Conflicts with other goals were implicitly modelled by varying chain state transition probabilities, each of which are functions of the environmental context, physiological state and the patient’s technical therapy setup.
Conclusions
Our novel simulation environment extends physiologic models with a holistic description of interaction between patient and decision support system. The simulation environment blends behavioral and physiological aspects which allows us to validate prototypical solutions in-silico early on.
USE OF DO-IT-YOURSELF HYBRID CLOSED-LOOP IS ASSOSICIATED WITH BETTER GLUCOSE MANAGEMENT AND HIGHER QUALITY OF LIFE AMONG ADULTS WITH TYPE 1 DIABETES
Abstract
Background and Aims
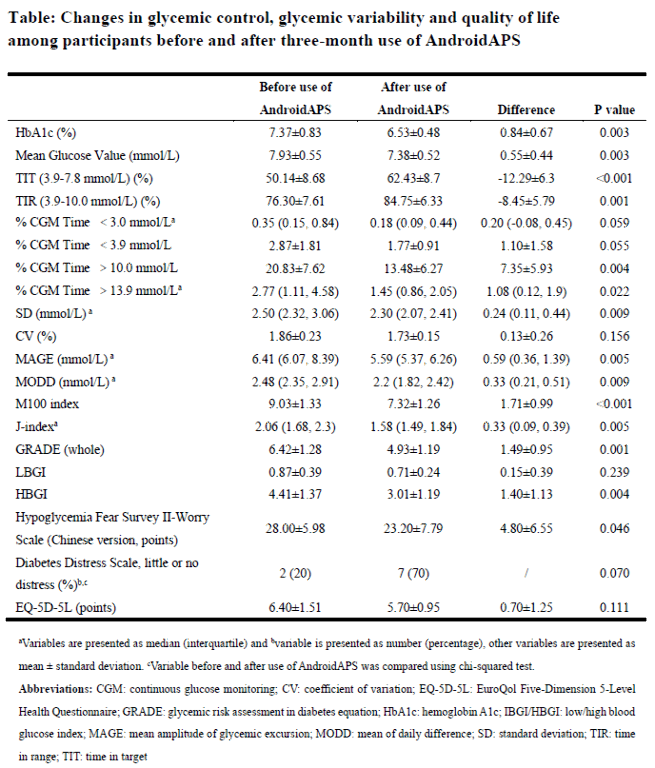
Previous studies show that do-it-yourself hybrid closed-loop (DIY-HCL) is associated with better glycemic control, but were largely biased by usage of estimated hemoglobin A1c (HbA1c) in the analyses. We aimed to assess the effect of using one of the DIY-HCLs, AndroidAPS among adults with type 1 diabetes (T1D) with documented data.
Methods
This was a retrospective study, approaching participants with T1D who reported self-use of AndroidAPS from T1D China Registry Study. We included those met criteria below into analysis: aged >18 years; having complete record of ≥three-month continuous use of AndroidAPS (version2.0 enabling super micro bolus and un-announced meal features, with Bluetooth-enabled continuous glucose monitoring systems and pumps); with documented HbA1c and Quality of life (QoL) records before and after three-month use of AndroidAPS; and not pregnant. All included participants provided written informed consent. Pair t test or chi-squared test was adopted to compare variables before and after use of AndroidAPS.
Results
149 participants were screened and ten included in analysis (six female, median age:34.1 years [range:20.1-69.4], median diabetes duration:13.0 years[2.7-23.7], median HbA1c:7.3%[6.4-8.8]). Data of the first three-month of using AndroidAPS were analyzed, as shown in the Table. Use of AndroidAPS was associated with decreased HbA1c(7.37±0.83%vs.6.53±0.48%,P=0.003), prolonged time in target(50.14±8.68%vs.62.43±8.7%,P<0.001) and time in range(76.30±7.61%vs.84.75±6.33%,P=0.001), and less glycemic fluctuation. Lower level of fear of hypoglycemia was also observed after using AndroidAPS, together with seemingly less time in hypoglycemia(P=0.055). No severe hypoglycemia or diabetic ketoacidosis occurred.
Conclusions
Use of DIY-HCL was associated with improved glycemic control, glycemic variability and QoL among adults with T1D.
USER PERCEPTIONS AND SATISFACTION WITH DO-IT-YOURSELF CLOSED-LOOP SYSTEMS FOR TYPE 1 DIABETES
Abstract
Background and Aims
A patient-driven movement has been integral in developing do-it-yourself closed-loop systems (DIYCLS) for management of type 1 diabetes (T1D), in which insulin delivery is adjusted based on continuous glucose monitoring data. There is limited information on the use of DIYCLS and the benefits and challenges experienced by this patient population.
Methods
A cross-sectional survey was completed by users of DIYCLS. Participants were recruited through social media and a diabetes database platform.
Results
For the 180 participants, mean age was 34 years and mean duration of T1D was 20 years. The educational level was college degree or higher for 81.5%. Twenty-six percent of responses were for pediatric users, and 42.9% of respondents lived outside of the United States. The average self-reported hemoglobin A1c was 6.3%. Since initiation of DIYCLS, respondents reported decreases in hypoglycemia (86.5%) and hyperglycemia (87.6%), an increase in sleep quality/quantity (74.7%), and decreases in time spent managing T1D (69.4%) and in T1D-related stress (76.9%). Overall, 69.3% were very satisfied with DIYCLS, and only 1.8% were moderately or very dissatisfied. Participants were particularly satisfied with the systems’ handling of overnight blood glucose (97.6%). There was less satisfaction with ease of initial set-up and troubleshooting, with 19.9% and 19.3% reporting dissatisfaction, respectively.
Conclusions
Users of DIYCLS report overall satisfaction and perceive positive changes in terms of glycemic management and quality of life. The challenges experienced in set-up and troubleshooting are important to consider as further developments in closed-loop insulin delivery are expanded for all people living with T1D.
